Ischiofemoral Impingement Syndrome | How To Identify And Self Help
Medical jargon is sometimes as complex as a labyrinth. Arguably, ischiofemoral impingement (IFI) is one of these difficult terms. But once explained, it is no longer hard to understand.
If you have heard the term and need to know what it means, this article will give you the answer. But I’m not only here to demystify the tongue-twister. I’ll also share a few clues from my experience as a physical therapist to treat hip pain and solve the problem.
Did you know many patients get better with physical therapy and other conservative measures? I’ll explain further, but let us start with the basics.
What is an ischiofemoral impingement, and where is it located?

In an article published in the Journal of Hip Preservation Surgery, orthopedist Hans Gollwitzer defines ischiofemoral impingement as “a narrowing of the space between the lateral aspect of the ischium and the lesser trochanter of the femur with entrapment of soft tissue structures” (1). But cutting through the medical mumbo-jumbo, what does it mean?
Let’s picture the hip joint. There is a defined space between bones and other anatomical structures, which differs from person to person. Here, we refer to the space between the lesser trochanter and the ischium. That is a prominence of the femur and the surface of the hip bone.
Generally, this so-called ischiofemoral space measures 2 cm. It allows various muscles and nerves to go through without problem. Ischiofemoral impingement refers to a space reduction that triggers hip pain (2).
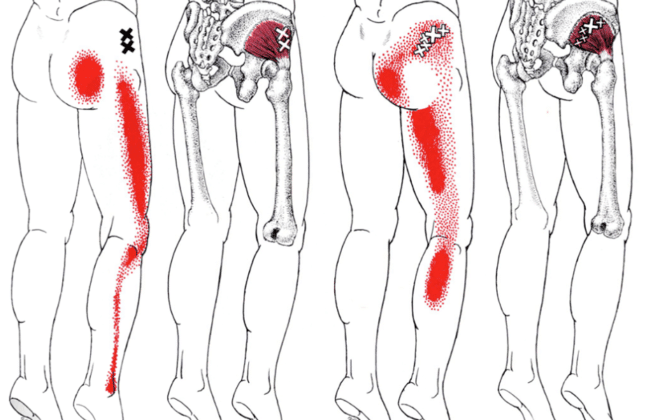
The space is not wide enough, presses the structures, and turns your buttock into a hotstop. Ischiofemoral impingement commonly causes sciatic nerve entrapment and affects other soft tissues. Therefore, it is considered part of the deep gluteal pain syndrome.
As we will cover, you can have symptoms that radiate to the leg when the nerve is affected. However, you’ll find the problem in the hip joint where the ischium and the lesser trochanter meet.
How does the ischiofemoral impingement work? What are the causes?
As mentioned above, ischiofemoral impingement consists of a reduction of the ischiofemoral space.
The extension of this space is dynamic. In other words, it can change from person to person and at any moment. It changes slightly with gait. However, it is usually around 2 cm (2).
Anything that reduces this space can cause an ischiofemoral impingement. For example, after hip replacement surgery the new joint may become slightly misaligned.
However, some people are predisposed to it because of the size of the lesser trochanter and other structures. Furthermore, we can have edema in the area, which causes pressure.
Let’s look at these and other causes, one by one.
Causes of ischiofemoral impingement syndrome
We can divide the causes of ischiofemoral impingement into primary or secondary. That is, congenital or acquired.
The former are inherent to the human body. These generally refer to deformities or anatomical variants. You can say they are your body’s original quirks. The second cluster is due to modifications of your anatomy or changes that occur over time.
Among the primary causes we have (3):
- Coxa valga. In this condition, we have a reduction of the angle between the neck of the femur and the bone shaft. Although minute, this change can reduce the available space between the bones.
- Position of the femur. When the femur is located slightly toward the center and back, the risk of ischiofemoral impingement increases.
- Pelvic bone anatomic variants. The pelvic bone may also be slightly wider or protruding. When this occurs, the ischiofemoral space decreases. These variants are common in women. Therefore, women are more prone to ischiofemoral impingement syndrome.
Secondary causes include (3):
- Replacement surgery. This syndrome started getting attention in patients after pelvic surgery. When the components are slightly misaligned, they can obstruct or step on the nerve.
- Tumors. It is uncommon, but sometimes we can find a growth pushing on anatomical structures in the ischiofemoral space. It can be a lipoma or fatty growth.
- Overuse or trauma. It is a common trigger in athletes. Repetitive motion and overuse of the joint can cause pain. One of the mechanisms is edema. It features fluid accumulation in the area that pushes the structures and presses on the nerve.
- Functional disorders. If you have developed hip problems such as hip instability or problems with your abductor and adductor muscles, these can cause ischiofemoral impingement.
What are the symptoms of ischiofemoral impingement syndrome?
We can include the symptoms of ischiofemoral impingement syndrome in the deep gluteal pain syndrome, too. They are as follows (1):
- Posterior hip pain or buttock pain
- Pain may travel down the leg when the sciatic nerve is involved (radiating gluteal pain)
- Hip pain is usually worse when sitting for more than 30 minutes.
- Tingling or numbness in the affected buttock or leg
We may guess whether the cause of ischiofemoral impingement is primary or secondary. In young people affected in both hips, it is most likely a primary cause. In seniors with unilateral pain, the causes are most likely secondary.
Knowing this, you may have something to check on yourself before going for a consultation. However, keep in mind that everything you are reading is only informative.
You need an evaluation by a healthcare professional to identify the problem. Only then will you be able to get personalized advice after getting an accurate diagnosis.
How is it diagnosed?
The diagnostic process has different steps, including:
An exploration stage
It all begins by evaluating the symptoms, as described above. The patient’s age, previous illnesses, and the unilateral or bilateral nature of the problem can provide many insights.
Therefore, your therapist or physician may ask several questions. It is advisable to answer accurately and provide all the relevant data.
A physical exam
In addition, your therapist can identify the problem by physical examination. There are no validated clinical studies, but at least two are very effective to evaluate the ischiofemoral space. One of them is called the ischiofemoral impingement test, or IFI test. The other is known as a long-stride walking test (4).
- The IFI test consists of extending the hip in a lateral position with the hip in abduction. Your therapist will help you do this specific movement, so you don’t have to worry about it. It can be uncomfortable, but the discomfort is temporary.
- You also have the long-stride walking test. In this case, the examiner will ask you to walk with long strides.
In both cases, the test is positive when causing the characteristic pain of hip impingement.
A study published in 2016 by Gomez-Hoyos et al. showed that the IFI test has a sensitivity and specificity of over 80%. The long-stride walking test has a sensitivity of 94% and a specificity of 85% (4).
In other words, they are excellent for detecting the problem and ruling it out as a differential diagnosis.
Diagnostic imaging
The final step is diagnostic imaging. Imaging usually helps us rule out other problems. They do not necessarily provide the final word.
Ultrasound can identify edema, and radiography is useful to find bony abnormalities. On the other hand, magnetic resonance imaging (MRI) provides more data when all of the above provide insufficient data, for example, in the case of a quadratus femoris muscle tear.
Differential diagnoses
A differential diagnosis includes any other health problems we should rule out as they have similar symptoms. It includes all entities of the deep gluteal syndrome. For example, piriformis syndrome, problems with the iliopsoas tendon, hamstring tendon edema, and so on.
They all press the sciatic nerve and can have similar symptoms or the same. However, your therapist will be able to recognize them through a thorough physical examination.
Likewise, similar symptoms may be present in posterior hip arthropathy. Even ischiofemoral ligament sprain can mimic these symptoms.
This is why getting yourself evaluated with a physical exam is so important. Each muscle has a specific range of motion, and we can find out where the discomfort is coming from by reproducing the pain.
How is ischiofemoral impingement syndrome treated?
We can divide treatment into operative and non-operative. One requires surgery or an invasive approach, and the other does not.
The most recommended is the conservative treatment. It features anti-inflammatory drugs and exercises to beef up the core and hip abductors.
We can also use corticosteroid injections in the quadratus femoris muscle. This strategy serves to both diagnose and treat the problem. Some doctors may also use botulinum toxin. However, these injections are still experimental (1, 3).
On the other hand, surgical treatment aims to increase the distance between the lesser trochanter and the ischium. We can accomplish this through surgical decompression of the ischiofemoral space. For instance, with a resection of the lesser trochanter. Doctors can do it through an open technique or with endoscopy.
What conservative measures are used?
We have mentioned above two fundamental conservative measures to alleviate symptoms. One is the use of anti-inflammatory drugs. The other is specific exercises to strengthen the core and abductor muscles because they usually feature hip abductor weakness. Let’s briefly review them and a few others (3):
- Most symptomatic patients benefit from anti-inflammatories. These medications help reduce quadratus femoris muscle edema and free up the ischiofemoral space. You can also contribute to this through your diet by consuming anti-inflammatory foods—for example, omega-3 and turmeric.
- Something else you can do is exercise, but in the right proportion and in the right way. Your therapist will tell you what exercise to include in your daily routine to improve your symptoms. These mainly strengthen the core and abductor muscles.
- If you are an athlete, one thing to consider is to avoid excessive exercise and heavy loads. Remember that hip joint overuse can also cause ischiofemoral impingement syndrome.
- When you walk, try to stay at ground level. Uneven surfaces and hiking trails can trigger the problem.
But above all, don’t hesitate to call your therapist or doctor if you experience a flare-up. Remember that this guide is no more than a starting point. If you follow instructions from a professional you may in time improve your quality of life. And doing so does not necessarily require surgery.
References:
- Gollwitzer, H., Banke, I. J., Schauwecker, J., Gerdesmeyer, L., & Suren, C. (2017). How to address ischiofemoral impingement? Treatment algorithm and review of the literature. Journal of Hip Preservation Surgery, 4(4), 289-298.
- Torriani, M., Souto, S. C., Thomas, B. J., Ouellette, H., & Bredella, M. A. (2009). Ischiofemoral impingement syndrome: an entity with hip pain and abnormalities of the quadratus femoris muscle. American Journal of roentgenology, 193(1), 186-190.
- Gómez-Hoyos, J., & Martin, H. D. (2019). Ischiofemoral Impingement. Posterior Hip Disorders: Clinical Evaluation and Management, 215-228.
- Hatem, M. A., Palmer, I. J., & Martin, H. D. (2015). Diagnosis and 2-year outcomes of endoscopic treatment for ischiofemoral impingement. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 31(2), 239-246.
Sam Visnic
Most Popular Posts
Categories
- Deep Gluteal Pain Syndrome (8)
- Deltoids (2)
- Foam Rolling (2)
- Glutes (9)
- Hamstrings (5)
- Hypnosis for Pain (3)
- Lats (2)
- Levator Scapulae (4)
- Lifestyle (8)
- Massage Therapy (39)
- Mobility (21)
- Movement and Exercise (19)
- Muscles (22)
- Nutrition (2)
- Obliques (1)
- Pain (25)
- Pectorals (3)
- Piriformis (3)
- Plantar Fasciitis (11)
- Psoas (11)
- Quadratus Lumborum (3)
- Quadriceps (2)
- Rhomboids (3)
- Sciatica (1)
- Serratus Anterior (1)
- SI Joint (14)
- Sternocleidomastoid (1)
- Stretching (18)
- Subscapularis (1)
- TMJ (2)
- Trapezius (1)
- Uncategorized (12)