Gluteal Tendinopathy | Identify And Fix
Dealing with relentless butt pain? If you’re experiencing lateral hip region pain, it could be gluteal tendinopathy.
The buttocks are very complex structures. They contain many gluteal muscles and tendons. But none of these should cause lateral hip pain or discomfort after sitting for only a few hours.
What is gluteal tendinopathy? It is the medical name for the damage to the tendons of the buttocks, which can trigger deep gluteal pain. You can even get sciatica pain from gluteal tendinopathy.
But how do you know this is what you’re experiencing? Is there anything you can do about it? Does physical therapy help? You’re in the right spot to find the answer.
What are the symptoms of Gluteal Tendinopathy?
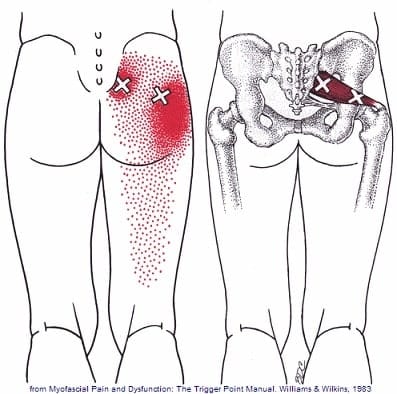
The main symptom of gluteal tendinopathy is pain, which is located laterally. This lateral hip pain starts mild and worsens over time. You may localize the pain in one side of the buttocks. It is unilateral (1,2).
It usually occurs in people who frequently carry weights or in runners. Thus, the pain increases with specific movements and loads.
If you have lateral hip pain, your therapist may use palpation to look for signs. They may touch the area above the great trochanter, which may cause pain or discomfort.
In many cases, the examiner asks patients to tie their laces. In gluteal tendinopathy, this movement triggers the pain (3).
Lateral hip pain may also leave you with other problems. For instance (1,2):
- Pain increases when you sit on the problematic side.
- The symptom may force you to sleep on one side only.
- Climbing stairs, walking, prolonged standing, or running may worsen the symptoms.
- Prolonged sitting triggers lateral hip pain, especially when sitting cross-legged.
- After prolonged sitting, you may experience difficulty walking.
What parts of your body does gluteal tendinopathy affect?
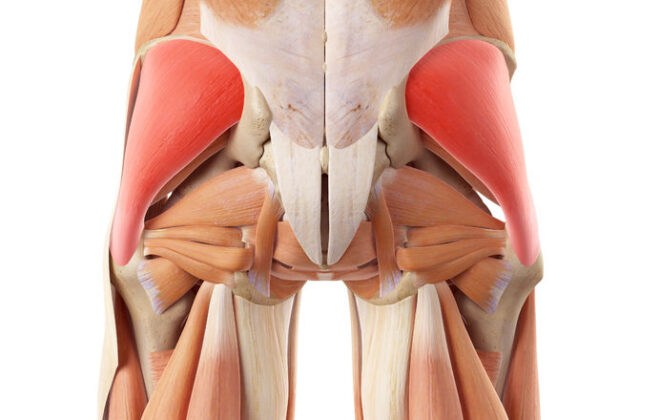
As the name suggests, gluteal tendinopathy affects the tendons of the buttocks. Two tendons are mainly involved. These are the gluteus medius tendon and the gluteus minimus tendon.
In this case, both gluteal tendons are affected by non-inflammatory processes. The most common include compression and overuse damage.
We can find these muscles in the gluteus. Still, patients usually report pain in the lateral hip. That’s where you have the tendon insertion (1).
What are the common causes of gluteal tendinopathy?
The gluteal muscles and surrounding structures are designed to withstand pressure. If that’s the case, why does gluteal tendinopathy affect some people and not others?
There are several possible causes. It usually involves a non-inflammatory event affecting the gluteus medius or gluteus minimus tendons. For instance:
The position of the joint
Researchers have found that hip adduction is a frequent pain trigger. In other words, when we bring the legs close together.
An example would be sitting with our legs crossed for a long time. Another example is keeping your knees together while standing up.
Maintaining this position while performing weight-bearing tasks can cause lateral hip pain. It’s because the iliotibial band compresses the gluteal tendons (4).
When holding a specific posture
Some postures promote compression on the gluteus medius and gluteus minimus tendons. Compressing them causes gluteal tendinopathy.
For example, when you stand on one leg. This position forces the abductor muscles and the iliotibial band to maintain pelvic control. These structures become tense and cause strain and compression in the gluteal tendons (1).
Some anatomical variants
Some people have a different angle between the neck and body of the femoral bone. These people may experience more tension in the iliotibial band.
This occurs mainly in women. They also have a small insertion of the gluteus medius tendon. Thus, the load of the iliotibial band won’t have an extensive surface to dissipate and it will be more likely to trigger pain (1,5).
What’s the difference between gluteal tendinopathy, gluteal tendinitis, and trochanteric bursitis?

Gluteal tendinopathy is a potential cause of deep gluteal pain syndrome. This syndrome brings together signs and symptoms found in other problems in the same area. Each one can have a different treatment.
That is why therapists need to highlight the differences between them. For example, how is gluteal tendinopathy different from tendinitis and trochanteric bursitis?
Gluteal tendinopathy vs gluteal tendinitis
The main difference between them is the source of pain.
In tendinitis, the cause is inflammation. We can locate this inflammatory process within the structure of gluteal tendons. Alternatively, an external structure can be the trigger. Besides pain, patients have edema (liquid retention) in the gluteus muscles (6).
In gluteal tendinopathy, the cause of pain is generally unrelated to inflammation. Instead, it is due to mechanical compression. As noted above, it can be due to an anatomical variant or the position you typically adopt.
Gluteal tendinopathy vs trochanteric bursitis
Similar to gluteal tendinitis, trochanteric bursitis is an inflammatory process. It is enclosed in the greater trochanteric pain syndrome.
In this case, the bursa is the source of the problem. This structure protects the hip joint. You’ll find the bursa above the greater trochanter.
Therefore, symptoms in greater trochanteric pain syndrome will be very similar but not the same. In trochanteric bursitis, the pain is located a little higher. Your physiotherapist can determine the exact location by palpation (7).
Other pathologies
Before diagnosing gluteal tendinopathy, it will be necessary to rule out other pathologies. For example, hip osteoarthritis.
X-rays are useful to make a clear difference. Your therapist may also suspect osteoarthritis with some maneuvers in the physical exam.
Many other health problems can also mimic gluteal tendinopathy pain. Thus, it is essential to rule them out with your examiner and ask as many questions as you may have.
What are the treatment options for Gluteal Tendinopathy?
Gluteal tendinopathy tends to get much better with physical therapy and some lifestyle changes. Some medical treatments and exercises are also available.
Here are some things you can do to relieve your pain (1,2,4):
Easy postural changes
Sometimes a simple change in your posture habits can improve your symptoms.
For example, avoid sitting cross-legged or standing on one foot. When sitting or lying down, do not put your weight on the affected side.
Build strength in your legs
Exercise therapy is essential for improving gluteal tendinopathy.
Many cases of gluteal tendinopathy are associated with atrophy and weakness of the gluteal muscles. By strengthening them, we also protect gluteal tendons.
However, you should ask your therapist for guidance. For example, some patients may need to avoid walking uphill, even if they want to strengthen their legs.
Maintain a healthy weight
Excess weight affects all the joints in your legs. The hips and buttocks are not an exception.
Maintaining a healthy weight will reduce the strain on your joints and help with gluteal tendinopathy.
Stick to your hormone treatments
If you have a hormonal imbalance, you should follow your treatment, especially as a woman. Gluteal tendinopathy pain can develop during menopause due to hormonal changes.
By addressing them and strengthening your legs, you can improve your symptoms.
Other treatment options
Besides these home measures, physical therapy and other treatments are also available.
The good news is that gluteal tendinopathy usually doesn’t require surgery. In most cases, conservative treatment is sufficient. For example:
- Oral therapy: like other types of pain, this can respond to painkillers. Over-the-counter analgesics are usually sufficient.
- Massage therapy: Trigger point massage, in particular, can help. This neuromuscular massage technique helps to identify tension points and release them through manual pressure. This technique should be applied by a physical therapy or massage specialist.
- Tendon rehabilitation techniques: Various exercises in physical therapy can rehabilitate gluteal tendons. You should perform these exercises under the instructions of your physiotherapist. They have a progression and will change as the condition improves.
- Other treatments: In some cases, a corticosteroid injection may be necessary to relieve gluteal tendinopathy. Shockwave therapy has also been applied. Surgery is recommended only when there is a tendon tear or when conservative treatment does not work. For example, in hip abductor tendon tears.
How long does Gluteal Tendinopathy last?
Symptoms of gluteal tendinopathy vary in duration, depending on the treatment used. It also depends on the severity of the tendon injury.
Many patients experience an improvement after three to eight weeks of treatment and/or rehabilitation. Again, it is necessary to follow the guidelines of your physician and physiotherapist.
Treatments such as corticosteroid injections may provide early relief. These usually have their peak effect by the sixth week. However, they are only temporary solutions.
Overall, the pain should not last more than a year. If it does, you are probably a candidate for surgical treatment, as it indicates that conservative treatment did not work.
But don’t worry. Most cases of gluteal tendinopathy respond very well to lifestyle changes and postural modifications. Physical therapy is also very effective, including exercise and massage therapy.
References:
- Grimaldi, A., Mellor, R., Hodges, P., Bennell, K., Wajswelner, H., & Vicenzino, B. (2015). Gluteal tendinopathy: a review of mechanisms, assessment, and management. Sports Medicine, 45, 1107-1119.
- Grimaldi, A., & Fearon, A. (2015). Gluteal tendinopathy: integrating pathomechanics and clinical features in its management. journal of orthopaedic & sports physical therapy, 45(11), 910-922.
- Fearon, A. M., Scarvell, J. M., Neeman, T., Cook, J. L., Cormick, W., & Smith, P. N. (2013). Greater trochanteric pain syndrome: defining the clinical syndrome. British journal of sports medicine, 47(10), 649-653.
- Grimaldi, A., Mellor, R., Hodges, P., Bennell, K., Wajswelner, H., & Vicenzino, B. (2015). Gluteal tendinopathy: a review of mechanisms, assessment and management. Sports Medicine, 45, 1107-1119.
- Birnbaum, K., Prescher, A., & Niethard, F. U. (2010). Hip centralizing forces of the iliotibial tract within various femoral neck angles. Journal of Pediatric Orthopaedics B, 19(2), 140-149.
- Paik, N. C. (2014, June). Acute calcific tendinitis of the gluteus medius: an uncommon source for back, buttock, and thigh pain. In Seminars in Arthritis and Rheumatism (Vol. 43, No. 6, pp. 824-829). WB Saunders.
- Redmond, J. M., Chen, A. W., & Domb, B. G. (2016). Greater trochanteric pain syndrome. JAAOS-Journal of the American Academy of Orthopaedic Surgeons, 24(4), 231-240.
Sam Visnic
Most Popular Posts
Categories
- Deep Gluteal Pain Syndrome (8)
- Deltoids (2)
- Foam Rolling (2)
- Glutes (9)
- Hamstrings (5)
- Hypnosis for Pain (3)
- Lats (2)
- Levator Scapulae (4)
- Lifestyle (8)
- Massage Therapy (39)
- Mobility (21)
- Movement and Exercise (19)
- Muscles (22)
- Nutrition (2)
- Obliques (1)
- Pain (25)
- Pectorals (3)
- Piriformis (3)
- Plantar Fasciitis (11)
- Psoas (11)
- Quadratus Lumborum (3)
- Quadriceps (2)
- Rhomboids (3)
- Sciatica (1)
- Serratus Anterior (1)
- SI Joint (14)
- Sternocleidomastoid (1)
- Stretching (18)
- Subscapularis (1)
- TMJ (2)
- Trapezius (1)
- Uncategorized (12)