Deep Gluteal Pain Syndrome MRI – What Can It Tell Us?
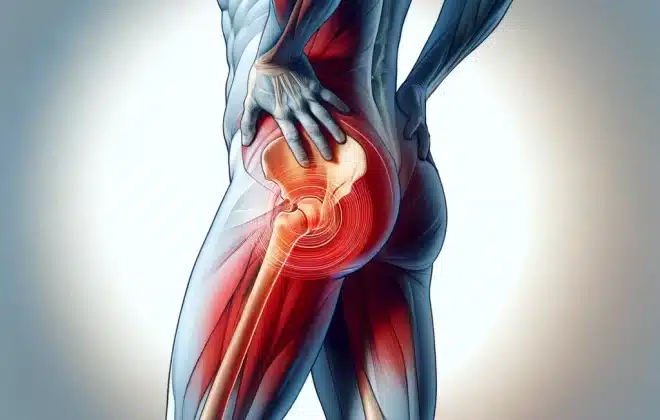
Deep gluteal syndrome (DGS) features symptoms such as pain after prolonged sitting, muscle weakness, posterior hip pain, among others. It can sometimes be problematic for doctors and physical therapists to unravel, not to mention patients.
Besides identifying the symptoms, professionals must dig into the deep gluteal space to find the root cause of the problem. This can be tiring for patients who constantly experience sometimes debilitating buttock, hip pain and sciatica symptoms.
But the diagnosis is a multi-step process. You’ll usually need confirmation after a physical examination with an imaging study. Magnetic Resonance Imaging (MRI) is the most commonly used tool by physicians to see what’s compressing or irritating the sciatic nerve, causing buttock pain and sciatic nerve entrapment. It is invaluable to investigate deep gluteal syndrome anatomy.
But, like other diagnostic tools, it can also have limitations.
How accurate is an MRI? Will it reveal the source of pain? What will happen after the study?
Stay around, and we’ll unpack the questions step by step.
Evaluating the Accuracy of MRI
MRI is essential in the gluteal syndrome anatomy imaging arsenal. But this clinical test is not a solitary act. In addition to the imaging study, a physical examination and a previous interview with the patient are paramount. All data collected forms the basics of the diagnosis.
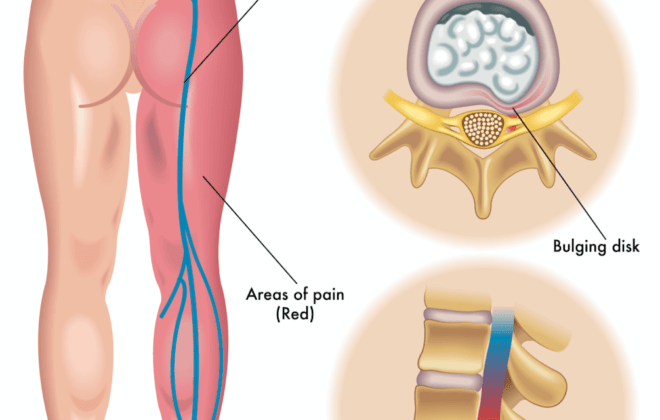
The first step of the diagnosis is examining the symptoms such as pain after prolonged sitting. Then, comparing them with an MRI identifies the location of sciatic nerve entrapment. But how reliable are the results of this study?
To answer this question, a team of researchers pooled 239 cases of sciatica of non-disc origin (meaning a disc issue was ruled out). They revealed a sensitivity of 64% and a specificity of 93% of MRI studies (1).
In other words, false positives are very uncommon with an MRI. But it also indicates a high incidence of false negatives.
Simply put, many patients could have deep gluteal syndrome anatomy issues, even if they don’t show up on their MRI. Thus, an MRI should confirm the diagnosis or rule out other causes. It is not a screening test.
MRI scans confirm a physical examination and the assessment of the patient’s symptoms. As a second step in the diagnostic process, the combination will yield the best results.
Adding to the arsenal, the new buttock pain and sciatica screening protocols include other procedures. One is known as response-to-injection study and the other is a sciatic nerve-specific exam. The former features an injection of corticosteroids and local anesthetics. The second involves the use of electromyography of the sciatic nerve.
This way it is possible to detect a non-discogenic sciatic nerve entrapment more accurately. It also narrows the search to the deep gluteal space. Altogether, this makes up the definition of the syndrome (2).
How does MRI results affect treatment?

Anatomy imaging and management often belong together to explore the most likely cause of your pain. It can be a piriformis syndrome, ischiofemoral impingement, or sciatic nerve compression. There are many other deep gluteal space problems, and MRI is an excellent aid to detect the trigger.
Depending on the MRI findings, we understand the cause of buttock pain. This shapes the treatment plan, which may include drugs or a physical therapy course. In some cases, doctors may even practice interventional magnetic resonance imaging to release entrapments in the subgluteal space.
So yes, the MRI can change the treatment approach. It can also guide the exercise course your physical therapist will implement in your case. Here are examples of how anatomy imaging and management meet in a clinical scenario (3,4):
Piriformis syndrome
MRI findings
Hypertrophy and some anatomical variants of the piriformis muscle can point to piriformis syndrome on MRI. A local anesthetic infiltration test can confirms these findings. It appears piriformis syndrome is the most common cause of deep gluteal pain.
Treatment
In this case, treatment usually consists of anti-inflammatory medications, muscle relaxants, and rest. Your physical therapist may recommend a 6-week course of exercises. If this approach does not ease deep gluteal pain, others may work better for piriformis syndrome. Botulinum toxin injection and surgical resection of the piriformis muscle are commonly used.
Variants of the sciatic nerve
MRI findings
Magnetic resonance neurography (MRN) show an abnormal course of the sciatic nerve inside the deep gluteal space. Around 16-17% of the population has this anatomical variant. Yet, not everyone will have sciatic nerve symptoms or any other clinical features. This may sometimes be included as a subtype of piriformis syndrome.
Treatment
In the presence of deep gluteal syndrome symptoms, the infiltration test may work as diagnosis and treatment. If this fails, an endoscopic tenotomy of the piriformis muscle is the treatment of choice.
Variants of the piriformis muscle
MRI findings
This is another subtype of piriformis syndrome. An anatomical variant in the deep gluteal space can also alter the interaction between the piriformis muscle and the sciatic nerve. For example, the insertion zone can be different, or we can have an enlarged piriformis muscle. This variant causes a misalignment of the anatomical components and may trigger deep gluteal pain.
Treatment
Pain may improve with physical therapy and other conservative treatments. But these sciatic nerve entrapments are usually more difficult to resolve. They will likely require an intervention such as endoscopic muscle resection to resolve sciatic nerve entrapments in the subgluteal space.
Deep gluteal syndrome triggered by trauma and overuse conditions
MRI findings
In these cases, MRI can also detect fibrous bands in the piriformis muscle. These adhesions form in response to inflammation. They push structures and cause sciatic nerve entrapment and deep gluteal syndrome.
Treatment
In this case, the most effective treatment is an endoscopic sciatic nerve decompression in the deep gluteal space.
Hamstring tendinopathy
MRI findings
MRI is also essential to diagnose deep gluteal syndrome triggered by the hamstring muscle. Hamstring tendinopathy is often associated with inflammation, which can be acute or chronic. The images may feature acute inflammation and edema affecting the sciatic nerve. In chronic inflammation, bands and fibrotic tissue form in the deep gluteal space.
Treatment
Many cases of acute inflammation have a successful resolution with physical therapy and other conservative treatments. On the other side, chronic causes usually respond only to surgery.
Other muscle-related problems
MRI findings
There are various nerve entrapment syndromes involving other muscles and deep gluteal structures. For instance, an MRI can reveal an ischiofemoral impingement syndrome. Other findings include edema associated with nerve entrapment or a muscle rupture.
Treatment
In these cases, nerve entrapment and sciatic pain are usually due to fibrous bands and scar tissue. Thus, the treatment of choice will be surgical debridement or neuroscopic endolysis to achieve sciatic nerve release.
What are the limitations of MRI in evaluating Deep gluteal pain syndrome?
As practical as MRI is, it also has limitations. Despite showing all the anatomical parts in detail, some of them escape the examiner’s view. It usually happens when the problem is associated with a movement, not with the anatomical structures in question.
Moreover, there’s also a psychosocial aspect of buttock pain. It can affect your quality of life to a great extent. Even if MRI shows nothing at all, you will probably want to do something about it.
We could describe at least two cases in which an MRI can miss the diagnosis:
- A type of piriformis syndrome involves a dynamic sciatic nerve entrapment. In other words, the sciatic nerve is only affected when adopting some postures or making some movements. The magnetic resonance neurography will not be able to detect cases of dynamic sciatic nerve entrapment. Sometimes MRI scans show edema associated with hyper-intensity in the sciatic nerve. But even so, the definitive diagnosis is made by endoscopy (4).
- Similarly, one of the main limitations of MRI has to do with orthopedic anomalies. When sciatic pain is triggered by orthopedic issues, these are not always visible on MRI. The neuropathy is activated in a specific position or during dynamic motion. Therefore, diagnostic images will often not capture the exact root cause of the problem (4).
As noted, all these diagnostic tools should guide and not replace clinical tests. A postural evaluation, a gait examination, and physical exam maneuvers can lead the diagnostic suspicion to a more accurate location. That’s how we make sure treatment covers the real cause of radicular pain and it will be much more effective.
Conclusion
Diagnosis and management of sciatic nerve entrapments often belong together. MRI is the most common tool in the gluteal syndrome anatomy imaging arsenal. It reveals problems in muscles, ligaments, tendons, and other structures.
However, other tools can complement and confirm suspicions. For instance, electromyography of the sciatic nerve and the response to treatment with corticosteroid injection or local anesthetics.
MRI stands out as one of the main approaches due to its 93% specificity. However, it has a sensitivity of 64%. In other words, abnormalities in these tests are unlikely to be wrong. However, there can be false negatives in many patients.
Moreover, piriformis syndrome can happen due to dynamic causes. There are also orthopedic triggers of deep gluteal syndrome (DGS). They are both unlikely to show up in an MRI. That is why it is a confirmatory tool and should not replace the careful study of symptoms and clinical tests.
The MRI will directly affect the treatment. In many cases of acute inflammation, rest, anti-inflammatory drugs, and muscle relaxants will do the work. In other cases, the patient will find relief with injections of local anesthetics in the deep gluteal region. Even when this doesn’t work, botulinum toxin injection and various surgical techniques can be an option.
MRI results may guide medical treatment and the exercises performed by your physical therapist. It’s a valuable tool to provide specific treatment but also has some limitations. Sometimes, immediate surgical treatment becomes a better option. However, in most cases, it is possible to resolve radicular pain with conservative treatment and physical therapy.
Sam Visnic
Most Popular Posts
Categories
- Deep Gluteal Pain Syndrome (8)
- Deltoids (2)
- Foam Rolling (2)
- Glutes (9)
- Hamstrings (5)
- Hypnosis for Pain (3)
- Lats (2)
- Levator Scapulae (4)
- Lifestyle (8)
- Massage Therapy (39)
- Mobility (21)
- Movement and Exercise (19)
- Muscles (22)
- Nutrition (2)
- Obliques (1)
- Pain (25)
- Pectorals (3)
- Piriformis (3)
- Plantar Fasciitis (11)
- Psoas (11)
- Quadratus Lumborum (3)
- Quadriceps (2)
- Rhomboids (3)
- Sciatica (1)
- Serratus Anterior (1)
- SI Joint (14)
- Sternocleidomastoid (1)
- Stretching (18)
- Subscapularis (1)
- TMJ (2)
- Trapezius (1)
- Uncategorized (12)