Simple Strategies to Live Beyond Chronic Pain
Lynne Wadsworth:
Thank you all for coming on another Living Life Naturally podcast and today we have Sam Visnic. He is here as our podcast guest and he spent his life studying the fundamental aspects of human health, but with a focus on movement and clinical massage therapy. So in a world of specialists, surgical procedures, drugs and quick fix remedies, he's committed to finding and developing strategies that help people stuck at the gap. So he has studied dozens of systems and methodologies for uncovering the root cause of aches and pains along with postural and movement issues.
Lynne Wadsworth:
So pain science and the art and science of hands-on soft tissue massage techniques, myofascial release, which I have been privy to and love it, and coaching movement is essential in his practice. So integrating different methods, but above all, deciphering way and to use different techniques with different people in situations along with the integration of movements that people want to be able to do again is the key to long-term success with Sam's incredible track record with his personal clients, excuse me, understanding the various elements that contribute to conditions and the power of communication and education makes his release muscle therapy program unique from other hands-on therapy approaches.
Lynne Wadsworth:
So I'm going to apologize ahead of time. We have storms here in Florida so I'm finding it hard to speak. So welcome to the podcast, Sam. We're so thrilled to have you here with us today.
Sam Visnic:
Thank you for having me. I'm very excited and congrats to getting through that long intro. You did very well.
Lynne Wadsworth:
So where are you joining us from today?
Sam Visnic:
Southern California in a town that is slightly east between Los Angeles and San Diego. It's called Temecula.
Lynne Wadsworth:
I have not heard of it and California is one of the few states I have not visited and I've been here over 30 years. Somewhere, I'd love to go, but of course at the moment in time, I'm not going anywhere.
Sam Visnic:
It's wine country here so it's a good destination spot.
Lynne Wadsworth:
Yes. Yes.
Sam Visnic:
If you like to drink wine and you like to golf, then this is a place to go to.
Lynne Wadsworth:
Yes. So tell us a little bit about what got you started in this field.
Sam Visnic:
Well, simply I was a fitness trainer. My teens, I was the classic stereotypical skinny kid that my parents and people told me, you need to go to the gym and lift some weights because you're too skinny. And from there, I got really interested in fitness and in particular, early on, I was always a kid that liked direction and rather than just showing up to the gym, I didn't know what to do so I would devour every book on fitness that I could and I ended up stumbling upon a lot of books. This was back when people used to go to Barnes and Nobles and Borders, there was no Amazon, and I would sit there and my mom would take me and I would sit there and read all those books. And scientific fitness books, scientific weightlifting books and I got a pretty early start into that.
Sam Visnic:
So when I was about 19, shortly after high school, I decided, I mean, "Hey, I could teach other people how to do fitness stuff," and I became a trainer. And first and foremost, when I started working at the gym, I started realizing, and this is when things in the early 2000s were starting to move toward this functional fitness thing. Everybody was starting to play with exercise balls and doing all sorts of things other than just sitting on the machines at the gym and everybody had something wrong with them. Had aches and pains, they had back problems, knee problems, and other trainers didn't feel comfortable working with them. They didn't feel good about it. They didn't know what they were doing.
Sam Visnic:
And I was at a point where I was confident in reading the materials that I was reading to take these people on. And what I found is, is that a lot of these cases, I was getting them better. People had been to a lot of doctors and therapists and they were cleared for serious, serious medical pathology but they had arthritis, they had back issues from time to time that were not really stable. They didn't feel good about it and I would get these people moving and doing squats and lunges and they felt better as a result. So I had realized I was onto something and now, everybody knows this. It's like, "Hey, go train your core and everything," but in the early 2000s that's not what the message was.
Lynne Wadsworth:
Right.
Sam Visnic:
And so, for probably that point forward for I've been at this now, so that's been about 21 years, I spent and devoted all of my time to reading everything I could get my hands on when it comes to corrective exercise movements and not only that, but the field in pain, in particular, has evolved dramatically in the last 20 years. So we know so much more about all of the aspects that affect chronic pain and chronic physiological issues. And I've been able to integrate that stuff into my practice as both basically a movement therapist and what we call a clinical massage therapist.
Lynne Wadsworth:
So why is it then that nowadays so many people are dealing with chronic pain? What's your take on the course for that?
Sam Visnic:
It used to be that I would say things like, for example, bad posture and not moving enough and so forth and these are certainly elements because those in the therapeutic process, when we get people doing these things, they start feeling better. But I don't believe that that's really and that's not what the research says is what's causing and contributing to chronic pain. A lot of this starts off with all the way back to the beginning when people first start feeling aches and pains and then what they do about them. So for example, there's a good amount of research that goes into, how do you know when somebody has an injury, let's say they roll an ankle or they lift a box or whatever and their back goes out, I don't really like that word, but we use that for our purposes. How do they respond in this situation and how does it go from a point where the issue should be healed? The tissue calms down, et cetera, but then the pain persists after this.
Sam Visnic:
This is the difference between acute pain and chronic pain and there are certain things that will increase the likelihood of there being a chronic factor to the pain. So a lot of times we go to the doctor, that's what most people do if something doesn't just resolve on its own. So they go to the doctor and say, "Hey, my ankle is messed up. I rolled it. It's swollen," or "My back doesn't feel good. What do I do? It's been killing me," and the medical professionals at that point, as usual, their job is to rule out clinical pathology that you know is serious. Do you have something significant wrong with your spine?
Lynne Wadsworth:
Right.
Sam Visnic:
Is something broken? And that's the way it's supposed to go.
Sam Visnic:
But the problem is, in many of these cases, these individuals are oftentimes getting x-rays and MRIs and all sorts of scans and so forth in non-serious cases. So these cases, when you come in with a typical garden-variety back problem, generally it should be, most doctors will say, "Hey, you're going to be okay. I don't see anything seriously wrong. I'll give you some anti-inflammatories, give it a rest and you'll be fine," or go to physical therapy. But now it's like, the first step is, "Well, my back hurts," and then, "Let's get an MRI," and then, okay, hold on a second. So we get an MRI and the statistics show that recently there was a study that showed, if you take a hundred people off the street and you run an MRI on them, on their spine, you'll find that somewhere in the neighborhood, 60% of them have some abnormality on the scan.
Lynne Wadsworth:
Wow.
Sam Visnic:
They have arthritis and this is all run at the middle stuff, that's normal yet. But now, the diagnosis is your back problem is because of this issue. So you have a disc bulge in your back that's why you have this pain. And now, because you're not explained things like, "Hey, everybody has this so I don't know if that's what's causing your pain. Let's give it a little bit of time. It's probably going to be okay," either you're told, "Hey, nothing's wrong with you," after you've been told you have a disc bulge; or number two, you're told that the whole problem is because of that but you're not explained the scenario on how you're actually supposed to fix this, right? Or what does this mean? Does this mean you have a bad back? Does it mean that... Whatever.
Sam Visnic:
And these are certain things right there that start to create fear. It creates anxiety. It creates concern that something could go wrong. And now, it starts to lead to certain beliefs like fear-avoidance, not wanting to do certain things with your back or let's say that you were playing something, a sport that you love like golf or tennis. You might now start becoming apprehensive about doing things because you feel there's something wrong with your body and you can get hurt. So now you could start to see how this chronic pain issue could start developing from now developing behaviors and beliefs that are associated to what just happened. And maybe you really just had a simple low backache and it was going to be fine after a little bit of rest and you could go back to doing what you're doing, right?
Sam Visnic:
So this is just a small scenario but an extremely common scenario that I think is one of the factors that can increase the chronicity of aches and pains. And it's not so much of like a blame on the medical system but this is just how things are going. And there's actually big movements in orthopedic societies now and trying to tell more common physicians to stop over x-ray-ing, over MRI-ing because it's number one, not that valuable in assessing and diagnosing common back issues, for example; and two, it overestimates the problem. It causes more people to end up being on medications. It causes more people to end up being on the surgical table when they don't need these things and increasing the likelihood of developing a chronic problem.
Sam Visnic:
But you've take it all the way back to there and there's many other factors, as people continue to see more doctors and therapists and they get more diagnoses and they end up not really doing well with the therapy, it causes people loss of hope. It causes more concern and worry about the situation and the whole thing snowballs and it continues getting people stuck in this what I call the vicious cycle of chronic pain.
Lynne Wadsworth:
Right. So many of us, it seems, especially here in the US, we hear so much about the chronic pain, it's ongoing. And I think that we really need to learn to be our own health advocates when we go to the doctor because, as we say, it's either underdiagnosed or over diagnosed
Sam Visnic:
Yes.
Lynne Wadsworth:
And we really have to go in there and really fight for ourselves these days.
Sam Visnic:
Yeah. And it's confusing because it's a medical doctor and their doctor is trained to detect serious issues. So there has to be a trust that that is happening but also, it has to be an understanding of where the expertise lies. And I would say that their specialty is not necessarily chronic pain, it's making sure nothing is seriously wrong with you. And some doctors are more knowledgeable on chronic pain and some are not. So I tell people, if you go in and you see your physician, tells you that they don't see anything wrong with you and you're stable, you know what I mean? Your structure is stable and whatever the issue is, there's nothing that's medically and emergency situation, as frustrating as that might sound, that's a good thing, because that means that now there are other things that we probably need to deal with that are not so serious in terms of a medical perspective.
Lynne Wadsworth:
So how do you know if one pain therapy is better than another when it comes to people that you see?
Sam Visnic:
That is a huge question and a good one because there are so many things out there and we're inundated, as usual, with marketing messages and so forth of everything that works. So what I do with people, and that's what I get lots of flurries of questions, does this technique work or does that technique work? Myofascial release or exercise therapy? To some degree, almost everything will work. The problem is, is understanding the totality of the situation that is happening with the person in their own, what we would call unique pain experience. There is no universal thing in every single situation of pain that is the cause of the pain, because if that was the case, we would already have the solution. We would know that every back issue would be fixed by doing core exercises or we would know that every jaw issue would be fixed by using a bite guard and it does not work like that.
Sam Visnic:
Anybody who works with patients will find that there's a certain amount of success by doing certain types of therapies. It's not always clear when a therapy will work. But I can say, and this is where the development of my release system is based upon years of researching certain things in particular with chronic pain, we know that certain therapies or certain things that we do in the process will increase the likelihood of having a success with more different types of therapies, okay? So let me explain that. So we know now that after a lot of research that teaching people about pain, okay, because most people don't have any idea what pain really means in the body other than, in the short term, if you burn your hand on a hot stove, you look at your hand, well, you know why it hurts. That makes sense.
Lynne Wadsworth:
Right.
Sam Visnic:
We can square that up. We don't need a lot of understanding to understand that. But when we have chronic pain, which means that the tissue has healed, the burn is healed, but we still have pain, we don't understand that because that doesn't make sense. And we need people to understand or to help us understand the process of why those nerves are still sensitive after the tissue has healed and imagine dealing with that situation for years. Your hand is now producing pain when there's technically nothing wrong with it. That's very frustrating. So we know that when let's say a neurologist or a physical therapist or somebody comes in and explains to you why this is happening and why those nerves are sensitive and what you can do about it, first and foremost, that gives you a little bit of relief. It gives you some hope, "Oh, I understand it now. Somebody gets this."
Sam Visnic:
So when I work with people, I always start with pain education. I teach people about chronic pain and all of the different factors that are associated to it. And to help them understand that when we start to go through our process, we're going to be digging a little bit to see which factors are involved that they weren't even aware of, right? Because oftentimes people, when they come into me, me, as a massage therapist and a movement specialist, they're looking for a mechanical fix. It's posture, it's movement, there's something very particular in there and there may absolutely be components of that, okay, and it's almost always, to some degree, but there are many other factors outside of that that will influence your ability to respond to those therapies. So to give an example, we know that pain education, if you don't understand what's going on in your body, let's say that you do believe you've been diagnosed previously with a disc bulge that if you bend forward, you're going to hurt your back.
Sam Visnic:
So if I give you exercises that involve bending, you're going to have apprehension and you're going to have fear about doing those movements and you're going to start generating nervousness and/or pain without that movement actually being something that is painful. So if I explain to you about pain and how it works and that the disc bulge is not really an issue and it's common, and what we're doing is desensitizing your nervous system to these movements that are very safe and controlled, you're going to respond differently to that therapy at that point. So it literally can be the difference that makes all the difference. So pain education, one. Some other factors that we might look at in the research that... There's mounds of research on this and that's why I like to talk about especially things that have been really, really validated that don't actually get talked about very often.
Sam Visnic:
One of the number one things that increases your sensitivity and your nervous system to pain is how well you sleep. If your sleep is poor, then you will respond in a greater way or too much, I would say, to small amounts of stimuli. So if you get an exercise that makes it ache a little bit, right, but you generally feel, okay, let's say you have two nights of bad sleep, now that exercise might make you hurt a lot. And then you go to the therapist and you say, "Hey, these exercises are making me hurt. I don't want to do this," but really it wasn't the exercise. It was the state of the nervous system. So the more you understand about what's going on in your body and all of these factors, it makes it easier to navigate this process of desensitizing those nerves, getting the nervous system to restore its normal state of homeostasis and getting the results that everybody wants which is to move past the chronic pain and get back to living their life.
Lynne Wadsworth:
Yeah. Because living with chronic pain is absolutely no fun whatsoever. I'm a migraine sufferer so I totally, totally understand where people are coming from when it comes to chronic pain. And I used to not understand what the doctors would say when they would tell me, "Oh, this is chronic," but definitely there are so many factors. And tell me if you don't agree with this, but as a holistic health coach, there are so many factors, as you say, you mentioned just one with sleep. But there are many others that affect how we feel and how we might respond to that chronic pain. So I think that some of what you do is that you deal with people when it comes to behavioral changes as well.
Sam Visnic:
Yeah. And you have to, in a general way, and this is where things get interesting with selecting therapies. Almost every person who comes in, almost, I'd say, has dabbled with certain therapies that we know are helpful, for example, meditation. But I can't tell you how many people I've seen that are habitual meditators, that meditate on a regular basis, they're good with having it at a routine but it's not helping their chronic pain. And that's because if there's generalized stress in someone's life and they're always responding and overreacting to all different types of stressors then a generalized meditation routine is very helpful because it will, to some degree, improve their coping. It's probably also stopping them from getting worse. But that pain has a specific experience and it's very contextual and that meditation might need to be applied in a very particular way to the context in which that person experiences pain in order for them to get better.
Sam Visnic:
So I hear a lot of, well, meditation doesn't work and I'm an advocate of medical or more clinical hypnotherapy, for example. I've tried that, that doesn't work. What do you mean it doesn't work? And with whom and under what circumstances? Because if you were just given a generalized relaxation routine, maybe that didn't work for you but maybe you have fear about bending forward like we talked about. But if that meditation or that hypnosis is not acting on the specific fear about bending forward, it may not work because it's not specific enough to the individual, right, and their individual pain experience. So yes, you've got all of these factors and that's what makes it challenging because we would love to just go in and flip someone's life upside down overnight and make every area of their life better but we know we can't do that and in that in particular stresses people out.
Sam Visnic:
So we have to try to, as best we can, hit the nail on the head the first time if we can and that's great when that happens, but we don't want to set those expectations. But we oftentimes have to test and that's why that good interview process on the front end and doing a quality evaluation and asking a lot of questions can help us narrow down the specific context in which those behavioral outputs are actually occurring. Meaning, when does the pain happen and under what circumstances? What's going on in your brain when you do this? What are you thinking? How are you moving? All of these contextual elements and we're going to have a greater likelihood of being successful by targeting our therapy without having to necessarily just keep circling around it with therapies that are good in terms of general health, but they may not be dramatically impacting the pain itself in the way that it needs to be impacted.
Lynne Wadsworth:
So you have talked about massage. So what kind of massage do you do with your patients? I'm assuming it's not always the traditional type of massage.
Sam Visnic:
No. So for me, massage of all types is good. Like I say, that massage is very much like pizza, even when it's bad, it's good. Because even when someone's nervous system is stressed out, if you're so stressed and you've got all this stuff going on, sometimes just lay it on the table and doing massage therapy is just fantastic. It'll calm the nerves. I don't do that work. I oftentimes refer that out. But when people come to see me for specific massage work, I have a number of techniques that are designed to basically change what we call the sensory experience of the issue that needs to be dealt with. So when I do an evaluation with somebody, we do always do a head to toe because no body part works in an isolation. If some muscle group or group of muscles or an area where there's pain, let's say the shoulder, if those muscles are tight and locked up, then what are all the muscles around it doing in response to that?
Sam Visnic:
They have a behavioral change as well to do what they're doing for compensation purposes. So you create a blueprint of all of the muscles that are tight and the muscles that are loose. So the massage work is going to be very specifically targeted to that area, right? So we're going to go through, and most of the time, my work is all about, I say thoroughness. So you'll find that for the most part, when people have gotten massage therapy, I've had clients who've gone to renowned experts and clinics and so forth. And by the time they get to me, I always ask, has anybody really gone through your shoulder and cleaned out and worked on every single muscle that attaches around that ball and socket? And 99% of the time they say, "Nope, nobody's ever done that before," so that's where I'm always going to start.
Sam Visnic:
I'm going to go through it, usually, let's say on a shoulder, it will take me an hour and I will literally go through every strand of muscle fiber and see how sensitive things are, how's the person responding to that. If they have a reduced range of motion, let's say I work on that muscle, does anything change? I'm always looking for doing some kind of therapy and retesting to see improvements. In that way, I don't have to deal with treating that entire shoulder every single time they come in. I could jump ahead to the parts that make the most significance and when I do that, I'll use a lot of different techniques. And in massage therapy, all of the massage therapists to some degree have played with a lot of different techniques whether or not they have a branded name associated to them or not, that depends on what it is, but I use a bunch of them.
Sam Visnic:
If I were to say what I use the most, it's probably myofascial release techniques and also something that's called muscle energy techniques which is a system of doing contract-relax activities to improve range of motion in the joints, in the tissues and improve that sense of safety that the person feels when they move their joints around.
Lynne Wadsworth:
Because nowadays, so many people spend the majority of their time on the computer and so many of us, therefore, as a result, have neck pain, shoulder pain, back pain, as you're talking about it in here.
Sam Visnic:
Yes.
Lynne Wadsworth:
So do you find that you can address that to where it can be taken care of and then they can maybe continue to do exercises to keep that area released? Or is it like a few months that you have to work with people? How does that work?
Sam Visnic:
Yeah, that depends on how many things are contributing to that. So I don't find that sitting or this whole concept that text neck is really that much of a problem because I always loved that, in the physical therapy community, always produces these funny memes that antagonize some of these beliefs sometimes. For example, I think the famous one that goes around is a black and white photo of people going to work on the subway in the '40s or the '50s and they're all standing there looking down at newspapers. So they had newspaper neck, right? But I don't think that that's the problem. I think what the problem is, is being stuck in a position for too long without moving. I think that's the primary problem.
Sam Visnic:
So I'll always start with things like how long are you sitting without moving? Are you literally static and focused which is a good thing because you're working, but you've got to remind yourself to wiggle around in your seat and move without just being stuck in one plane of motion with your eyes moving. Your neck is going to have some stiffness when you start to move it.
Lynne Wadsworth:
Right.
Sam Visnic:
So a lot of times, it's producing activities outside of the chair that are antagonizing those positions. So if you're like this, we're going to do lots of exercises that do the opposite. We're also obsessed in the culture of movement and chronic pain like physical pain with stretching. And not that stretching is bad, but it doesn't last, right? So what we want to do is whatever muscle is tight, I oftentimes go right away to exercising the opposite muscle because if my shoulders are going up, they're tight, but what are the opposite muscles doing? They're lengthened.
Sam Visnic:
So what I'm going to do is do exercises where they pull their shoulder blades back and down to make those muscles stronger so that they antagonize the tension in the muscles that are tight. So then, you're stretching will actually probably last a little bit longer when you do that. So I always go with that but also we assume that muscles that are tight actually are strong and a lot of times they are not. A muscle can be tight because it's strong, it could be tight because it's weak. And for the individual, you have to determine that but that strategy is actually when you figure that out leads to the long-term success.
Sam Visnic:
So human beings are meant to move. We need to move a lot, but we need to have a strategy. So outside of just stretching, are we going to exercise those muscles to make sure that they have a good ability to tolerate sitting in that position for as long as the person needs to sit? And that's what we say is the concept of improving functionality. That's what's important, is getting somebody to be able to tolerate what they do all day long with less discomfort and problems.
Lynne Wadsworth:
So tell us a little bit about the book that you have because I know that you have written a book yourself.
Sam Visnic:
Yes. So what I had done over the years is I'd always be finding myself telling people things and without spending my time with clients, lecturing them constantly on all of the findings that I've found throughout the research, I decided to create a digital version of my book and put all of that stuff in there. So I'd help people understand as a compendium and say, what is chronic pain and what does the research say about this and what is all this stuff you hear me babbling about in sessions? And I want you to read it, learn about it and understand what I say when I say that fixing posture is not the only thing that's related to pain and actually far from it. What does the research say about orthotics and all these questions that people would love to have answered and the common ones.
Sam Visnic:
And I just wrote the digital copy of the book and sorted it to chapters to talk about the various things. And a lot of it is pretty mind blowing to people when they read it. And then particularly talk about things like core exercises and just strengthening your core, we hear so much, does not work for back pain at all. There's no research to support it. And people are like, "Really?" Because I hear that all the time. Yes. And the more you understand about what's out there in terms of there's a lot of research supporting, and then you see where things are starting to go, you'll understand a lot more about what I'm talking about in terms of why we educate people. Because the more you understand about pain, the better you feel, the more we start not obsessing about structural biomechanics and your posture, the more it releases you, gets you to relax a little bit more and the more it brings some calm to your nervous system and that in response reduces pain.
Sam Visnic:
I also talk about things like hypnotherapy, which mark my words, I'm now, as I'm doing my podcasting tour here, talking a lot about, mark my words, that will be the next thing. The only thing that we have to overcome here when it comes to meditation and hypnotherapy is the stigma that's associated to them. There's mounds of research to support why hypnotherapy works. One of the major researchers on this is Mark Jensen out of University of Washington that finds that these processes like hypnotherapy and meditation, although they're different processes, they work the same way on the brain and what they do is they calm the brain. And the brain is the thing that is predominantly choosing or deciding whether or not you should experience pain or not which is really the threatening response that our body has when it's getting information that tells us we're in trouble.
Sam Visnic:
So the more we work on the brain through these various processes, the more we calm things down and the more we can restore a normal, healthy function. So I talk about these things in the digital book and it's my gift for people because there's just so much information out there. A lot of it is misinformation and people are led in the wrong direction, spending lots of time, money, and energy doing things that are just not supported and I personally found in my practice that don't work either. So that's what I'm offering out there to help people along.
Lynne Wadsworth:
And where do they find that?
Sam Visnic:
They could get it directly on my website. So if you go to my homepage, at releasemuscletherapy.com, and you scroll down to the bottom of the page, it's a bundle of a free membership area that I have on my website with a lot of different resources. And I write a few PDFs, small eBooks, and so forth to help people understand how to use some of these techniques right away to start noticing a difference and restore balance to their nervous system.
Lynne Wadsworth:
Awesome. So what general recommendations can you give to our listeners that would actually help them get better now?
Sam Visnic:
Yes. There's four pillars to dealing with chronic pain. There's a lot of details in these, but four general pillars to getting better from chronic pain. Number one, pain education. The more you understand about pain and there's research to support this, that when they put people in MRIs and we look at how much their brain activity they have when they're in pain, because we can't measure pain, by the way. We can only measure stress responses to that stimuli. There's a lot of brain activity going on when people have pain. And when you educate people with pain education and you stick them back in the MRI machine, you notice a much quieter brain. So actually education itself is therapeutic just by learning. So pain education is number one, okay? The number two thing is you need to sleep. You need to improve your quality of sleep, however that means for you. Get to bed on time, don't drink too much water, don't drink tons of caffeine, whatever you need to do. Get help from an expert on sleep.
Sam Visnic:
The number three thing is you got to move and not necessarily talking about right away core exercises or anything else, but we find that general aerobic exercise, just getting out walking reduces the likelihood of having issues with anxiety and depression associated with chronic pain and also helps getting some fitness, right? So getting out, breathing air, right? As long as it's nice outside.
Lynne Wadsworth:
Right.
Sam Visnic:
Right? Yeah. And then the last thing is goal setting and this is a big topic and a can of worms to bring up about why we set goals. Pain relief itself cannot be the only goal of a therapeutic program. It has to be about improving function. And what I always say is that there's this paradoxical thing that occurs which is the more you fixate on pain, the more pain you experience because you make your nervous system pay more attention to it.
Sam Visnic:
The brain will always pay more attention to what you teach it to pay attention to. So when we look at those small improvements, "Hey, I got some sleep yesterday. I feel a little bit better today. I went on a little bit longer walk," or "My goal is to go to the gym and actually just spend 20 minutes in there, just moving around, lifting some weights. I did that and I couldn't do that before." The more of this information and input we're putting into our nervous system with these small goal improvements, we're sending lots of information that shows our nervous system that we are safe. And when we're safe, that alarm, i.e. pain starts to ratchet it's way down, okay?
Sam Visnic:
So that is the four pillars. So we have pain education, we have sleep, we have some extra movement and we have goal setting. And those are the things that you can start implementing right now to improve your situation.
Lynne Wadsworth:
Well, Sam, that's so helpful. I appreciate that. So tell our listeners, I know you've told us your website, but tell us again where people can find you.
Sam Visnic:
Yep. Go to releasemuscletherapy.com, that is my home site and, of course, feel free to go to my Instagram. I always keep updated content. Not everybody goes and reads blogs all the time these days but it's on Instagram. It's /releasemuscletherapy. You'll see lots of exercises and information that I put out there so you can keep updated with me. I'll be launching my own podcast here pretty soon-
Lynne Wadsworth:
Wow.
Sam Visnic:
... In which I'll be interviewing some experts that I love to hear about and a lot of it is, I have to be honest, I'm a little guilty of saying it's really some self-serving part for me because I have lots of questions that I want to ask the experts that I interview and I want to learn a lot. And everybody will get to go along for the ride and I love to poke at them and ask them a lot of deep questions to get past some of the superficial stuff.
Sam Visnic:
So those are the things that are on the docket for me and reach out any time, I offer virtual consulting and so forth. But my mission is really helping people out of this chronic pain cycle because it is vicious. And the good news is, that it is not as hard to break out of as most people actually think that it is because oftentimes they've been through so much and it has not worked for them. But let me tell you something, there is a light at the end of the tunnel because there is a lot you probably have not done.
Lynne Wadsworth:
That's awesome. Thank you so much. Appreciate you being here with us today and giving us all of this valuable information.
Sam Visnic:
Yes.
Lynne Wadsworth:
Very, very helpful. Thanks.
Sam Visnic:
And thank you for having me on here. I really enjoyed it.
Lynne Wadsworth:
Thanks. So till next time, enjoy California. Hope that your weather stays well, good, and the health of the Californian stays well.
Sam Visnic:
Yes, indeed. It's heading on into the fall here. So especially in Temecula, maybe we'll get some sub 100 degree days.
Lynne Wadsworth:
Here in Florida, we're just looking forward to getting rid of the humidity.
Sam Visnic:
Good luck with that.
Lynne Wadsworth:
Yeah. Thank you again. Appreciate you being here with us.
Sam Visnic:
Thank you.
Lynne Wadsworth:
Bye for now.
Tags In
Sam Visnic
Most Popular Posts
Categories
- Deep Gluteal Pain Syndrome (8)
- Deltoids (2)
- Foam Rolling (2)
- Glutes (9)
- Hamstrings (5)
- Hypnosis for Pain (3)
- Lats (2)
- Levator Scapulae (4)
- Lifestyle (8)
- Massage Therapy (39)
- Mobility (21)
- Movement and Exercise (19)
- Muscles (22)
- Nutrition (2)
- Obliques (1)
- Pain (25)
- Pectorals (3)
- Piriformis (3)
- Plantar Fasciitis (11)
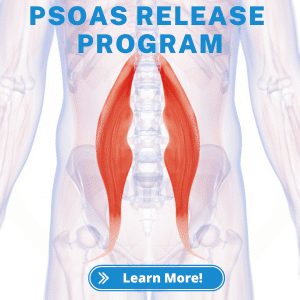
- Psoas (11)
- Quadratus Lumborum (3)
- Quadriceps (2)
- Rhomboids (3)
- Sciatica (1)
- Serratus Anterior (1)
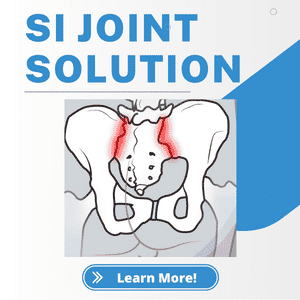
- SI Joint (14)
- Sternocleidomastoid (1)
- Stretching (18)
- Subscapularis (1)
- TMJ (2)
- Trapezius (1)
- Uncategorized (12)