Sensitization In Chronic Pain: Knowing This Changes Everything
 Over the past decade, more scientific data has been made available to explain challenging cases of chronic pain that appear resistant to any generally accepted and appropriate therapeutic approach.
Over the past decade, more scientific data has been made available to explain challenging cases of chronic pain that appear resistant to any generally accepted and appropriate therapeutic approach.
A new theory that is gaining acceptance is central and peripheral sensitization. It's a process that contributes to various types of pain syndromes, including things like fibromyalgia and osteoarthritis.
As you will see in this article, central and peripheral sensitization has been found to be responsible for unexplained changes in pain caused by both biomechanical and other triggers.
Knowing about these phenomena can be an absolute game-changer for people with chronic pain that no one can seem to figure out or help them with.
The role of central and peripheral sensitization
Different from many other organs, the brain undergoes continuous changes, known as neuroplasticity. These changes are responsible for learning, but they also modulate excitability and neuronal activity.
Central sensitization is a modulatory process in the brain that results in a persistent state of high reactivity. In this state, the pain threshold is lower, and individuals may still feel pain after an injury has already healed.
On the other hand, peripheral sensitization is often a cause of central sensitization, and it is modulation or change in the peripheral nervous system that disrupts pain perception, and is perceived by the brain as a constant source of pain.
This is a common finding in cases of nerve injury, both mechanical and chemical. Thus, central and peripheral sensitization may be responsible for various forms of pain that cannot be explained by a biomechanical model, as in ghost limb pain and fibromyalgia.
The type of pain triggered by central and peripheral sensitization has two main characteristics, known as hyperalgesia and allodynia.
Hyperalgesia is an exaggerated perception of pain after a stimulus that is mildly painful, such as slight pinpricks.
Allodynia refers to experiencing pain with stimulus that is not normally painful, as in simple touch or gentle pressure.
Individuals experiencing unexpected or random shifts in pain sensation are not crazy or making up their symptoms. That same goes for those who sometimes experience improvements after taking medications, doing movement, or getting a massage, but at other times are extremely irritable as a result of these same things.
Still, we cannot generalize and say that ALL types of pain come from central and peripheral sensitization. In most cases, they are no more than pain modulators that contribute to noxious stimuli and sometimes explain the maintenance of pain symptoms in otherwise healthy people.
Mechanisms of central sensitization in chronic pain
The changes and modulation of pain pathways in cases of central and peripheral sensitization are very subtle and difficult to detect. In most cases, they will be changes in the receptors at the molecular level inside whats called neuronal cells.
These changes occur after repetitive activation of pain receptors. These changes in brain connectivity are coupled with changes in neurochemistry, in particular an increase in the release of chemicals that are associated with pain perception.
Thus, we will have abnormal levels of GABA, choline, and glutamate, which have been correlated with a bad mood and increased perception of pain.
There are a few potential causes of central sensitization:
- Stroke: It causes chemical and structural modifications in brain tissue, leading to altered pain perception in some individuals.
- Spinal cord injuries: This leads to structural modulation of pain pathways, and it is responsible for unexplained causes of pain after trauma.
- Genetic factors: There appears to be a genetic prevalence as a predisposing factor for central sensitization. None has been found yet, but it appears to be the case according to the scientific data.
- Stress and anxiety: Negative emotions have a profound effect on the neurochemistry of the brain, and can promote a state of alert that triggers excitability and favors the perception of pain.
- Prior history of psychologic or psychiatric ailments: Anxiety, traumatic memories, depression, psychosis, and similar ailments maintained for long enough can create dysregulation in the neurochemistry of the central nervous system that may trigger central sensitization.
- Poor sleep: It is a cause and consequence of pain, and acts as a vicious cycle, increasing sensitivity to pain at the same time.
As noted, pain perception is much more than biomechanical impulses. It has a strong biopsychosocial aspect that we should be aware of.
The most logical approach to dealing with chronic pain
Even though the understanding of central and peripheral sensitization is available for everyone, and has a pretty solid foundation, many healthcare practitioners don't appear to be well-informed of these mechanisms and may not take them into consideration when working with an individual suffering from chronic pain.
The focus is often almost exclusively on biomechanical causes of pain, rather than realizing the value of the biopsychosocial aspects of health as they relate to the PERSON that has the pain.
Several therapeutic recommendations have been synthesized to improve chronic pain in individuals with central and peripheral sensitization.
- Exercise: Aerobic based physical activity, such as walking, light strength training, swimming, and even yoga can be helpful. They improve psychological symptoms such as depression and anxiety, and contribute to strengthening muscles. This is important for addressing any potential biomechanical sources of stress in the body. Interestingly, even individuals with irritable bowel syndrome can improve their symptoms and quality of life after following a 12-week exercise intervention!
- Cognitive-behavioral therapy: It is extremely important to educate people about pain (pain science education!), and techniques to cope with it. Cognitive-behavioral therapy can help relieve emotional responses to pain episodes, and help control the severity and frequency of symptoms. Even individuals with biologic causes of chronic pain, such as pelvic pain due to endometriosis, have reported improvements in quality of life after using cognitive-behavioral therapy in combination with alternative health therapies.
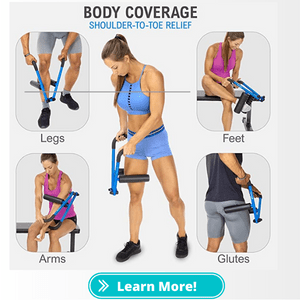
- Massage: Relaxation massage and/or bodywork which emphasizes reducing excess muscle tension can have profound effects on the chronic pain sufferer, even if only for the short-term. Research shows the effectiveness of massage therapy on symptoms such as anxiety and depression.
- Nutrition: The value of anti-inflammatory nutritional guidelines, eating for optimal blood sugar regulation, and attaining recommended daily intakes of certain vitamins and minerals is often under-emphasized. Food allergies, sensitivities, and nutritional deficiencies should be evaluated and addressed in the chronic pain sufferer in order to reduce overall physiological stress load.
So, in conclusion, recognizing central and peripheral sensitization in the chronic pain sufferer can immensely change the focus of the therapeutic approach health practitioners take to help the individual improve not only pain levels, but also quality of life. It's clear that focusing purely on the biomechanical model is insufficient and will fail to address the primary underlying issues involved. As always, a multi-disciplinary, biopsychosocial-based, TEAM-approach is best when it comes to working with chronic pain!
References:
Eller-Smith, O. C., Nicol, A. L., & Christianson, J. A. (2018). Potential mechanisms underlying centralized pain and emerging therapeutic interventions. Frontiers in cellular neuroscience, 12, 35.
Fleming, K. C., & Volcheck, M. M. (2015). Central sensitization syndrome and the initial evaluation of a patient with fibromyalgia: a review. Rambam Maimonides medical journal, 6(2).
M Adams, L., & C Turk, D. (2015). Psychosocial factors and central sensitivity syndromes. Current rheumatology reviews, 11(2), 96-108.
Ji, R. R., Nackley, A., Huh, Y., Terrando, N., & Maixner, W. (2018). Neuroinflammation and central sensitization in chronic and widespread pain. Anesthesiology: The Journal of the American Society of Anesthesiologists, 129(2), 343-366.
Lumley, M. A., Cohen, J. L., Borszcz, G. S., Cano, A., Radcliffe, A. M., Porter, L. S., ... & Keefe, F. J. (2011). Pain and emotion: a biopsychosocial review of recent research. Journal of clinical psychology, 67(9), 942-968.
Nijs, J., Van Wilgen, C. P., Van Oosterwijck, J., van Ittersum, M., & Meeus, M. (2011). How to explain central sensitization to patients with ‘unexplained’chronic musculoskeletal pain: practice guidelines. Manual therapy, 16(5), 413-418.
Woolf, C. J. (2011). Central sensitization: implications for the diagnosis and treatment of pain. Pain, 152(3), S2-S15.
Tags In
Sam Visnic
Most Popular Posts
Categories
- Deep Gluteal Pain Syndrome (8)
- Deltoids (2)
- Foam Rolling (2)
- Glutes (9)
- Hamstrings (5)
- Hypnosis for Pain (3)
- Lats (2)
- Levator Scapulae (4)
- Lifestyle (8)
- Massage Therapy (39)
- Mobility (21)
- Movement and Exercise (19)
- Muscles (22)
- Nutrition (2)
- Obliques (1)
- Pain (25)
- Pectorals (3)
- Piriformis (3)
- Plantar Fasciitis (11)
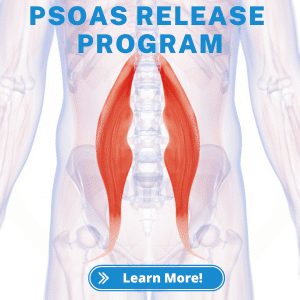
- Psoas (11)
- Quadratus Lumborum (3)
- Quadriceps (2)
- Rhomboids (3)
- Sciatica (1)
- Serratus Anterior (1)
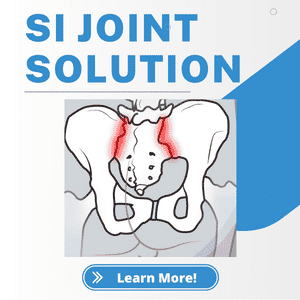
- SI Joint (14)
- Sternocleidomastoid (1)
- Stretching (18)
- Subscapularis (1)
- TMJ (2)
- Trapezius (1)
- Uncategorized (12)