Levator Scapulae Trigger Points | How To Identify And Self-Release
The levator scapulae, a vital component in the neck and shoulders functioning, plays a pivotal role in our everyday motions. Yet, it has the potential to transform into a cause of discomfort and pain.
Relief from problems like neck pain, stiffness, and even referred pain can be the result of identifying and resolving levator scapulae trigger points. Let’s take a look at this muscle, and how to locate these tender points, as well as effective techniques to resolving them.
The Levator Scapulae Muscle – Anatomy And Function
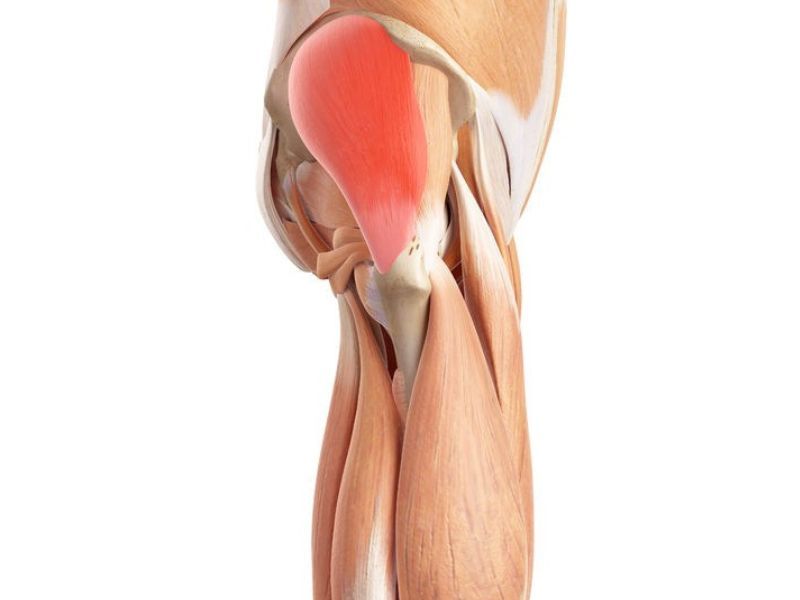
The levator scapulae muscle is a narrow, lengthy muscle that runs alongside and at the back of the neck. It originates from the posterior tubercles of the transverse processes of C1-C4 vertebras and inserts between the superior angle and the root of the scapular spine on the medial border of the scapula. The dorsal scapular nerve (C5) and the cervical nerves (C3-C4) innervate the levator scapulae muscle.
The levator scapulae muscle elevates the shoulder blade with the help of the trapezius and rhomboid muscles. These muscles also help to rotate the scapula downward by inferiorly tilting the glenoid cavity. This movement is essential for reaching overhead or behind the back. Additionally, the levator scapulae muscles assist with lateral flexion, neck extension, and neck rotation, which means bending and turning the head to the same side.
Trigger Points in the Levator Scapulae
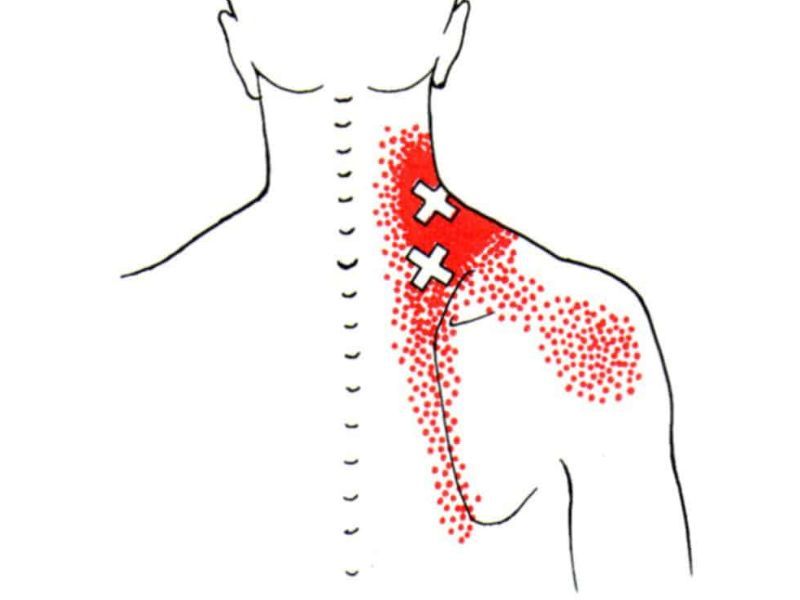
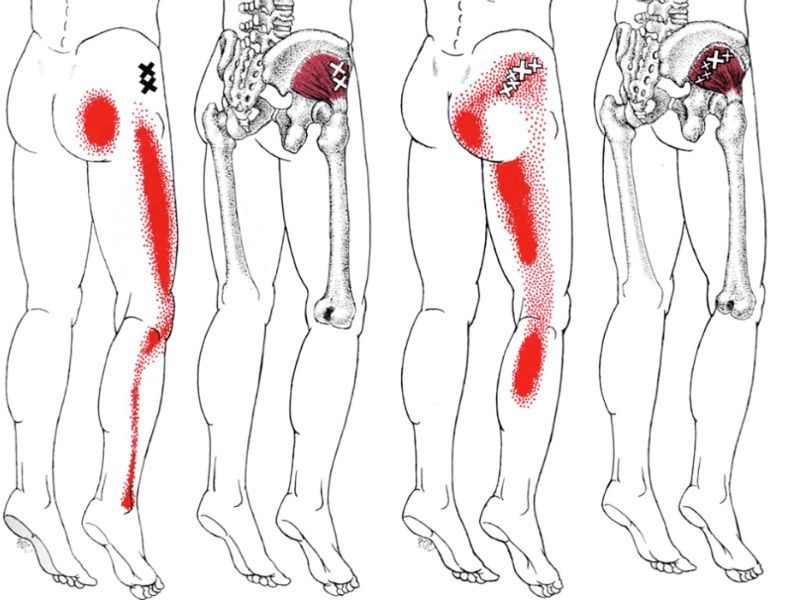
The levator scapulae muscle has two trigger points situated in its lower half. The lower trigger point is positioned just above the superior angle of the scapula, while the upper one is 1-3 inches above the lower trigger point. These trigger points are deeply embedded in the upper trapezius muscle and can cause pain that radiates laterally to the shoulder and along the inner edge of the shoulder blade. Movements such as elevating, rotating, or tilting the head or the shoulder blade can aggravate the pain.

Signs and Symptoms of Levator Scapulae Trigger Points
Some of the common symptoms associated with trigger points in the levator are:
- Pain in the neck region, possibly radiating to the head and resulting in a headache.
- Experiencing discomfort and limited range of motion, notably a decrease in the bending and tilting of the neck towards the opposite side.
- Deep, achy pain or tightness on the upper back along the top of the shoulder blade or neck.
- Increased trigger points and muscle tone.
- Difficulty sleeping or finding a comfortable position.
- Reduced breathing capacity or shortness of breath
What Causes Levator Scap Trigger Points?
A variety of factors can cause levator scapulae, including:
- Poor posture: Prolonged sitting, particularly with a slouched posture, can lead to a condition known as levator scapulae syndrome. This syndrome is often observed in office workers who spend extended hours seated, causing their shoulders and head to jut forward, creating a ‘hunchback’ position in the upper back and lower neck. Over time, this posture can cause stiffness and inflexibility in the affected joints. The persistent stress on the levator scapulae muscle reduces flexibility and chronic overuse.
- Carrying heavy bags with straps over the shoulder, such as backpacks, purses, or suitcases: The levator scapulae muscle could impact military personnel, particularly those who frequently carry heavy gear and engage in repetitive load-bearing tasks. These activities may compromise the upper body posture, potentially causing chronic stress or recurring injuries to the muscles and joints in the neck, including the levator scapulae.
- Stress, anxiety, or emotional tension can increase muscle tension and reduce blood flow.
- Repetitive arm motions (throwing, swimming, or racquet sports.)
Cervical spine dysfunction, such as disc herniation, osteoarthritis, or whiplash injury.
Treatment of Levator Scapulae Trigger Points
There are different treatment options for active trigger points, depending on the severity and duration of the symptoms, the underlying cause, and the individual preference. Finding out why there’s pain and fixing body movement problems that worsen it usually comes first. Some of the common treatment options are:
- Physical therapy: This involves hands-on techniques like massage, mobilization, or manipulation to release trigger points and restore muscle function. It also includes stretching and strengthening exercises to improve muscle length, enhance flexibility, posture, balance muscles, and prevent trigger point recurrence.
- Acupuncture: Acupuncture, a traditional Chinese medicine technique, has shown effectiveness in relieving pain, making it a valuable option for individuals seeking alternative therapies for scapula syndrome. Thin needles are strategically inserted into specific points on the body, stimulating energy flow and promoting the body’s natural healing processes.
- Local Corticosteroid Injections: For cases where inflammation plays a significant role in trigger point pain, corticosteroid injections offer a direct and powerful intervention. These injections aim to reduce inflammation around the scapulae muscles’ trigger points, providing relief from pain and promoting a more conducive environment for healing.
- Botox Injections: Botox injections present an innovative approach to treating levator trigger points. Botox temporarily paralyzes the muscle by injecting botulinum toxin into the affected muscle, leading to relaxation. This can be effective in cases where muscle tension significantly triggers point-related pain.
- Electrical stimulation: The levator muscle is subjected to a moderate-frequency current, inducing fatigue and sedation in the muscle, leading to a relaxation effect.
Heat or cold therapy: Heat or cold therapy relaxes muscles, boosts blood flow, and reduces inflammation and pain. Apply heat or cold to the muscle for 15 to 20 minutes, as needed. You can use tools such as a heating pad, hot water bottle, warm towel, ice pack, cold compress, or frozen towel.
Differential Diagnosis for Levator Scapulae Pain
Levator scapulae pain can be confused with other conditions that affect the neck, shoulder, or upper back, such as:
- Cervical radiculopathy: it occurs when a nerve compression or irritation in the neck causes pain, numbness, tingling, or weakness in the arm or hand
- Snapping scapula syndrome: In snapping scapula syndrome(washboard syndrome), the scapula rubs against the rib cage, resulting in pain and audible clicking or grinding sounds in the shoulder.
- Myofascial pain syndrome: This chronic condition affects muscles and connective tissues, leading to the development of trigger points. Research indicates that trigger points or myofascial pain syndrome can lead to heightened irritability in the muscle tissues, impacting the functionality of nerve endings and mobility.
- Cervical myofascial pain: A specific subtype of myofascial pain syndrome, cervical myofascial pain, targets the neck muscles. It results in trigger points, pain, stiffness, or reduced range of motion in the neck or head.
- Sternocleidomastoid syndrome: This condition appears as muscular spasms or trigger points in the sternocleidomastoid muscle, leading to discomfort, rigidity, or limitations in neck movement. Additionally, individuals may experience headaches, dizziness, or facial pain.
How To Self-Treat
Stretching the levator scapulae muscle can help lengthen the muscles and improve flexibility and posture. It also helps prevent or reduce muscle spasms, trigger points, and pain. Here are some levator scapulae stretching exercises that you can do at home or work:
Standing Levator Scapula stretches:
- Stand up straight, feet shoulder-width apart.
- Bend your chin down toward your chest and slightly to the right.
- Put your right hand on your head and gently pull down. You’ll feel a stretch on the left side of your neck.
- Hold for 10 seconds, then go back to normal.
- Do this 3-5 times, then switch sides.