Hamstring Tendinopathy | How To Identify And Manage
It can be a mysterious source of discomfort, especially in runners and other athletes. It can be the covert culprit behind a precipitous drop in physical performance. For many, it’s a little-known adversary causing chronic pain. It is often triggered by seemingly innocuous activities such as sitting.
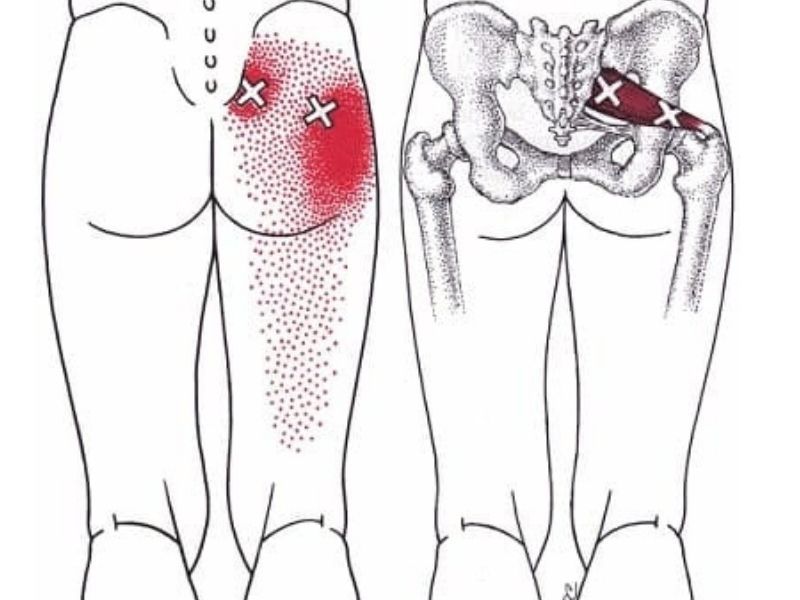
We’re talking about hamstring tendinopathy. This is an entity of deep gluteal pain and insidious discomfort associated with the sciatic nerve. But if you were recently diagnosed with this condition, many questions may arise.
What exactly is hamstring tendinopathy? How does your physical therapist diagnose and manage it? Is there anything you can do at home?
Let’s dive deep into understanding this pathology to answer these questions.
[lwptoc]
Understanding Hamstring Tendinopathy: Definition and Causes

The medical community initially recognized hamstring tendinopathy as hamstring syndrome in 1988. Since then, many athletes and seniors have been diagnosed over the years. It is common in runners, dancers, and endurance athletes.
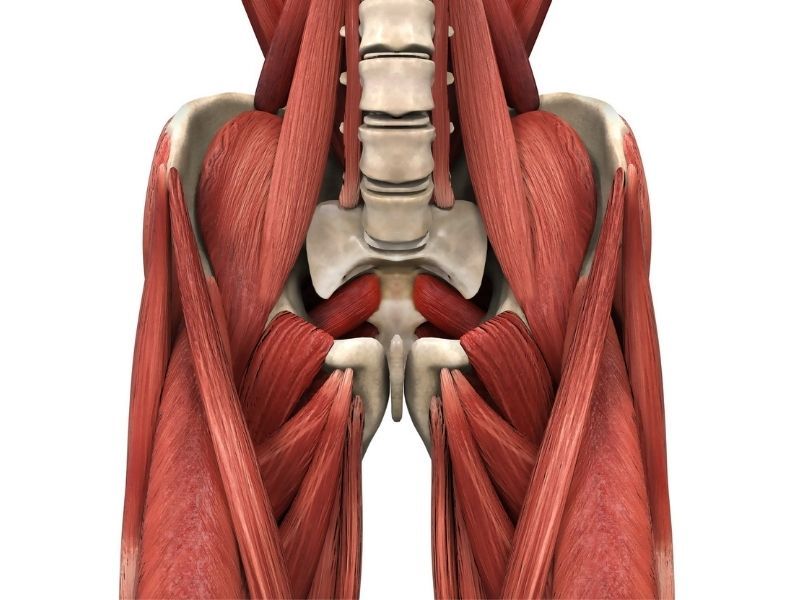
Hamstring tendinopathy occurs when hamstring injuries affect the soft tissue of proximal hamstring tendons. You will also find it as proximal hamstring tendinopathy (PHT) or high hamstring tendinopathy.
According to some authors, the formal definition is a lesion in the myotendinous junction of the hamstring with concomitant damage to the adjacent hamstring tendon, resulting in buttock pain, and pain in the posterior thigh, among other symptoms.
Surprisingly, up to 51% of dancers may encounter this problem. The primary cause? A muscle injury in the section where the hamstring muscle meets the tendon (1).
But why does it happen (1)?
- Overexertion: It may happen in sprinters at the terminal swing phase of the gait cycle. At that time, the hamstrings contract to decelerate the lower limb and can be subject to soft tissue injury.
- Active stretching: Hamstring tendonitis can also develop after active stretching of the muscle. This cause is less frequent and takes place in response to hip flexion with knee extension.
- Incorrect technique: It may also follow an overstretching move associated with sports. This may be the case in dancers or individuals attempting a high kick without the correct technique.
- Overuse & overload: Some authors also suggest overuse and overload hamstring injuries as possible causes. These more commonly affect the semimembranosus hamstring tendon.
Risk factors
In addition to the known causes, some risk factors increase the chance of proximal hamstring tendinopathy (PHT). For example:
- Older age.
- Reduced flexibility of the hamstring and quadriceps.
- Weakness of the hamstring muscle.
Some systemic factors may also influence the prevalence, such as:
- Diabetes.
- Hypertension.
- Obesity.
- Genetic predisposition.
Although the latter are not direct causes, they may contribute to proximal hamstring tendinopathy.
Spotting the Symptoms: Key Indicators of Hamstring Tendinopathy
The most notable symptoms of high hamstring tendinopathy are (1):
- Unilateral tendon pain in the posterior thigh or lower buttock.
- Neuropathic symptoms if the sciatic nerve is involved.
- Pain in ischial tuberosity worsens with repetitive contraction of the hamstring (uphill running, walking fast).
- Pain in ischial tuberosity worsens with direct pressure on the hamstring muscles when sitting.
- When sitting for long periods, patients may describe a boggy mass sensation around the ischial tuberosity.
- Symptoms develop gradually without a clear cause.
- In the case of avulsion hamstring injuries (a severe tendon tear), the tendon pain in the ischial tuberosity is sharp and very intense after trauma.
- In the above case, there may also be an audible popping sound at the time of trauma.
- Swelling may be seen in the tendon area in some cases.
Besides considering the symptoms of hamstring tendinopathy, how they came on, and where they radiate, your physical therapist will also look for signs. Signs are different from symptoms because your therapist can see and measure the health of your proximal hamstring tendons. They help detect proximal hamstring tendinopathy.
To that end, they will perform some clinical tests. These are maneuvers that may feel a bit uncomfortable, but they serve to identify the root of the problem (2).
These are available maneuvers your therapist may try on you (1,2):
Straight Leg Raise Test
This is an important test to examine the range of motion in proximal hamstring tendinopathy. It is an active assessment, meaning that the therapist will ask you to do it without help.
Keeping your leg straight, you should raise a single leg as far as possible. This will assess flexibility and whether the movement triggers hamstring tendon pain.
Slump Test
This maneuver is essential to identify radiculopathy in proximal hamstring tendinopathy. That is, to test if the sciatic nerve has been affected along with the proximal hamstring tendon. It is a neural tension test performed in a seated position.
The therapist will ask you to slump forward. If this does not cause pain in the ischial tuberosity, they will ask you to extend your knee as far as possible. A positive pain trigger means your sciatic nerve is likely involved.
Bent-knee stretch
This is a passive maneuver, in which the examiner will do the movement for you. The physical therapist will ask you to lie on your back on a stretcher.
They will take a single leg and bring your knee and hip to their point of maximum flexion and then slowly extend the knee. If this maneuver causes pain in the problem area, it is positive for proximal hamstring tendinopathy.
Modified bent-knee stretch
This maneuver is very similar to the previous one. It also requires the assistance of your therapist. Similarly, they will ask you to lie on your back. The examiner will take a single leg, flexing the knee and hip to the maximum, and then quickly extend the knee.
Similarly, the result is positive for proximal hamstring tendinopathy when this triggers pain in the ischial tuberosity. Some reviews describe this as the most sensitive and specific maneuver.
Puranen-Orava test
To perform this test, your therapist will ask you to stand up and keep your knee extended. The foot is placed on a support, raising it until the hip is flexed at a 90° angle.
It is positive for proximal hamstring tendinopathy if it reproduces the patient’s pain in the proximal hamstring area.
Hamstring loading movements
One of the main clinical tests involves load evaluation. This is done with different exercises focused on the hamstring muscle. The most common is the Romanian deadlift.
Tests are positive for proximal hamstring tendinopathy when they elicit the characteristic pain in the ischial tuberosity during exercise. To confirm, the therapist may decide to slightly increase the load, which also increases pain intensity.
Diagnostic Procedures
As with other causes of deep gluteal pain, high hamstring tendinopathy can be difficult to detect. Symptoms are often insidious at first. Because they are mild, inconsistent, and difficult to describe, many patients do not seek immediate consultation. And if they do, they often do not receive a proper diagnosis on their first attempt.
Basic assessment
In most cases, the pain is associated with mechanical loading of the hamstrings. It is almost always located in the ischial tuberosity. In most cases it does not change location or spread to other anatomical sites.
In the case of irradiation, this is usually due to a sciatic nerve entrapment. Almost always the radiating pain involves the hamstring muscles but rarely goes beyond the knee.
The hamstring tendon pain is aggravated by provocative activities. For example, running uphill, lunging, and during hamstring stretches. Even sitting can cause deep buttock pain, due to compressive loads across the hamstring.
All these data are important to have an initial diagnostic suspicion of proximal hamstring tendinopathy.
It is also important to check the symmetry of the lower limbs and palpate the ischial tuberosity and the proximal hamstring tendons.
Differential diagnoses
In some cases, imaging studies may be used to arrive at a diagnosis of proximal hamstring tendinopathy. This is not always performed in the setting of a physical therapist.
It is usually reserved for cases in which the tendinopathy does not respond to treatment. Also, when the specialist suspects another condition masks the symptoms of high hamstring tendinopathy.
In the diagnostic process, it is very important to consider differential diagnoses. These are other diagnoses with similar deep buttock pain or associated with hamstring tendinopathy.
One of the main conditions is sciatic pain. Any pain originating from the sciatic nerve can cause symptoms similar to hamstring tendinopathy.
Moreover, high hamstring tendinopathy is often complicated by neuropathy. Thus, although it is not automatically a deep gluteal pain syndrome, the possibility remains.
For the differential diagnosis of sciatica, your therapist may perform some maneuvers. For instance, the lumbar extension and flexion, straight leg raise, and slump test.
Similarly, it will also be important to test for the presence of systemic inflammatory disease. For example, psoriatic arthritis and ankylosing spondylitis (2).
Treatment and Management Strategies

Several treatments and management strategies exist for proximal hamstring tendinopathy. These include oral anti-inflammatory and analgesic medications, and targeted exercise. Other strategies include corticosteroid injections, platelet-rich plasma injections, shockwave therapy, and surgery.
Nevertheless, most people get better with conservative treatment. That is, most do not need surgery and other invasive treatments. Similarly, corticosteroid and platelet-rich plasma injections are rarely used.
The most important treatment and management strategies are as follows (2)
Patient Education
The main therapeutic tools available are education and exercise. Patient education is essential to identify the symptoms and their origin. This helps avoid recurrences in the future.
It is important to emphasize that pain does not always mean structural or biological damage. Patients and therapists can use pain intensity to measure advances. Pain determines how the proximal hamstring tendon functions and how well it can tolerate certain activities.
In this way, patients learn about their organisms, limitations, and precipitants throughout the treatment of proximal hamstring tendinopathy.
Rehabilitation
Focused hamstring muscle rehabilitation is also important. The usual rehabilitation period is three to six months. However, some patients may need longer rehabilitation, up to 12 months.
From an early stage, the programmed exercises aim to provide a load to the hamstring muscle-tendon unit in a progressive manner. From exercises with low load to exercises with higher load.
The individual patient’s response to deep buttock pain will determine what type of exercise to use, and what the progression will be. Pain symptoms are assessed 24 hours after exercise to make modifications to the intensity of the next exercise.
Some athletes begin with heavy slow resistance training. A senior by comparison requires starting with very low loads.
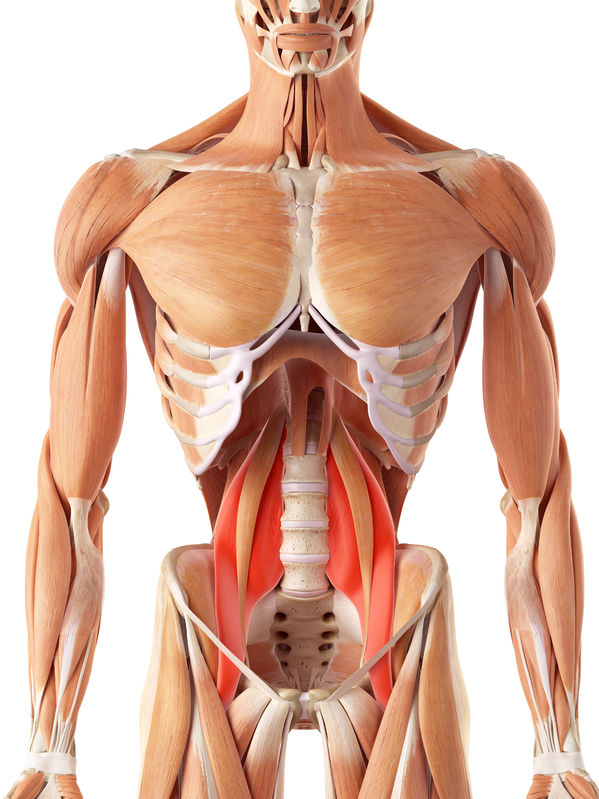
In some cases, it will also be necessary to rehab other muscles, as in an ankle sprain, triceps surae wasting problem, or any other injury in the past.
Rehabilitation also takes into account biomechanics. These can increase the load on the hamstring muscles and tendons. For example, we may need to correct the femoral-pelvic position, the anterior and posterior pelvic tilt, or an excessive forward trunk inclination, among others.
As the exercises progress the intensity increases in different ways:
- Incrementing the load
- Accelerating contraction speed
- Extending the hip flexion range
- Incorporating more complex exercises.
- Other conservative interventions
Other conservative measures
Besides performing these exercises and their evaluation, there are also passive interventions for proximal hamstring tendinopathy. These involve movements guided by an expert or manual therapy.
Corticosteroid injection therapies may also work but are best avoided, and platelet-rich plasma injections are becoming more of a popular trend.
Massage therapy is widely used in the early stages, and may help in getting the proximal hamstring tendon into the correct position. This is especially true is the work is neuromuscular therapy or myofascial release, which is far more specific than generalized massage.
Return to sports and prognosis
A concern in athletes is the return to sports quickly. In most cases, athletes will be able to continue their activities while completing their rehabilitation. Only your specialist can make that decision after examining your case.
Rushing rehabilitation is a common mistake, especially given the competitive nature of sports.
Prognosis is also a frequently asked question, especially about sitting pain. But sitting pain may improve over time, and can often take up to a year to be completely resolved.
Recovery will be more difficult in patients with other associated diseases, and athletes who rush to return to the playing field.
Surgical treatment
When conservative treatment does not work, surgical treatment may be necessary. In most cases, it consists of nerve debridement and release of the proximal tendon. Likewise, if there are any bands between the nerve and the hamstring tendon, doctors can remove them in surgery.
Tips for Preventing Recurrence
Despite treating tendon pain, one of the problems of high hamstring tendinopathy is the potential for recurrence. Some studies have reported up to 30% recurrence in cases of hamstring strain.
It is even theorized that tendon tears and damage to hamstring muscles cause changes in the long-term architecture of the hamstring tendon. It leaves a scarred section that replaces the normal fibers and tendons (2).
Thus, hamstring tendinopathy pain may return after some time, or have relief and reoccurrence periods. Some retrospective studies even show that more than 50% of patients with high hamstring tendinopathy experienced recurrences and failed to have a complete long-term symptomatic resolution (1).
Here are some recommendations to avoid a recurrence (1,2):
- Strengthen the hamstring muscles. This is one of the most important recommendations. The best prevention is working out the hamstring muscles according to their strength and endurance. The nordic hamstring curl is a super popular, although extremely challenging exercise for athletes.
- Strengthen the entire kinetic chain. That is, all the muscles associated with hamstring function. These muscles, even if they are accessory, relieve the hamstring load and decrease the risk of recurrence.
- Resolve deficits from past injuries. Often a past injury can be a trigger for high hamstring tendinopathy. If the injury is not resolved, the pain will return sooner or later.
- Avoid the use of corticosteroids. Although helpful in preventing or relieving pain, corticosteroids can lead to a greater recurrence of symptoms. This does not happen with other injections such as platelet-rich plasma.
- Ongoing evaluation. Even if you feel recovered from hamstring tendon pathology, it is essential to continue visiting your therapist. Only in this way will you be able to determine the actual degree of muscle recovery beyond the reduction in pain. They will also assess the limits of functionality to which you must adhere.
References:
Argo, L. R., Selley, R. S., Tjong, V. K., & Ihm, J. (2021). Proximal Hamstring Tendons. In Tendinopathy: From Basic Science to Clinical Management (pp. 103-127). Cham: Springer International Publishing.
Nasser, A. M., Pizzari, T., Grimaldi, A., Vicenzino, B., Rio, E., & Semciw, A. I. (2021). Proximal hamstring tendinopathy; expert physiotherapists’ perspectives on diagnosis, management and prevention. Physical Therapy in Sport, 48, 67-75.