Exercise is often recommended for many different health conditions, especially those related to the cardiovascular system, but it’s certainly not the only area where it may be extremely valuable.
Exercise is often recommended for many different health conditions, especially those related to the cardiovascular system, but it’s certainly not the only area where it may be extremely valuable.
Living a sedentary lifestyle is a fairly significant risk factor for health issues, and it not only limited to stroke and heart disease.
Chronic pain is included in the list of reasons to recommend physical activity, and even though many people are apprehensive of being more active when they have pain, studies show that it works and improves symptoms both in the short and long-term.
There are two main forms of physical activity (aerobic and anaerobic), and each of them is associated with an improvement in chronic pain.
We’re going to focus on aerobic exercise (often referred to as “cardio”), and how pain mechanisms can be inhibited by this simple form of movement.
During aerobic exercise, the most significant changes involve the respiration and cardiovascular systems. Your muscles play an essential part, and the stroke volume of your heart increases to make up for the increased requirement of oxygen and nutrients.
Thus, the function of your capillaries is enhanced, and the part of your cells that produces energy, called mitochondria, increases in both number and efficiency.
Additionally, there are many nervous system and hormonal adaptations that occur after aerobic exercise. These changes improve both strength and stamina, and have the ability to reduce insulin resistance and other metabolic problems.
Aerobic exercise can also play a role in improving flexibility, balance, coordination, and also positively impact muscle/postural asymmetry.
All of these improvements can be associated to various pain inhibitory mechanisms we’ll discuss below.
The exact mechanism by which physical activity improves chronic pain symptoms is not entirely understood. Unfortunately the vast majority of clinical trials do not make a clear distinction between aerobic and anaerobic physical activity when examining the effects of exercise on pain perception.
Most of these studies are a combination of interventions, therapeutic recommendations, and patient education, which makes it even more difficult to set aside and evaluate the differences between aerobic and anaerobic exercise separately.
That said, it is still possible to make a distinction based on what we do know by looking at the short and long-term effects of aerobic exercise.
Reduction of pain perception, called hypoalgesia, has been reported after physical activity in healthy individuals, people with chronic pain, and experimentally-induced pain.
There are two mechanisms involved in this short-term numbing effect: one of them is the release of endorphins, and the other is a modulation in the pain pathways in the central nervous system.
According to studies, after high-intensity aerobic exercise, there’s a hypoalgesic (numbing) effect lasting approximately 30 minutes. This effect is longer compared to resistance training exercise (anaerobic exercise), which lasts only a few minutes.
Studies seem to show that more exercise or a higher intensity is related to more hyperalgesia. The suggestion is that to generate a considerable effect we should engage in high-intensity physical activity for more than 10 minutes or moderate to high physical activity for 30 minutes or more.
Now of course you can imagine this wouldn’t work in a number of scenarios. For example some clinical trials have reported an INCREASED pain response instead of pain inhibition in cases of individuals with severe chronic pain.
People with fibromyalgia, for example, do not have immediate pain inhibition after physical activity, but of course they can still benefit from exercise in the long run.
The long-term pain inhibitory effects of aerobic exercise are only reported in individuals that maintained a regular program of activity.
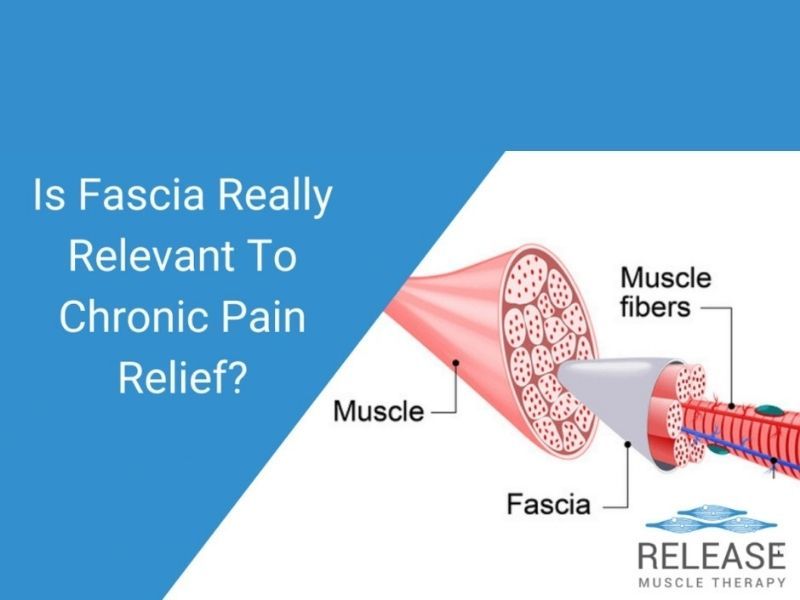
Long-term activity is known to modulate the endocannabinoid system (natural cannabis-like molecules produced by the human body), reduce the inflammation by improving circulation, and normalize transmission of glutamate in the brain and pyruvate in the muscle tissue.
By altering the release of inflammatory substances and improving circulation, it is possible to reduce swelling and other symptoms that may be associated with some chronic pain issues.
The endocannabinoid system in particular has a strong inhibitory effect that’s commonly targeted by pain medications. This system is also modulated by aerobic activity after releasing endorphins.
Additionally, glutamate and pyruvate are essential for sensory perception in the muscle tissue and its transmission in the central nervous system. Thus, by reducing these substances, physical activity may modulate pain perception in the long-run.
We can’t talk about pain perception without including the psychological function. It is well established that depression, anxiety, and similar mental health problems have a negative impact on pain perception.
Individuals that engage in aerobic exercise usually report a significant improvement in mood and psychological symptoms, which may have a positive effect on the chronic pain experience. There are not, however, enough studies to evaluate these changes in a large amount of people suffering from chronic pain.
In a nutshell, aerobic exercise is known to reduce pain perception immediately after exercise and in the long-run. However, for long-lasting results, it is necessary to engage in sustained activity, and most cases of chronic pain would also benefit from combining some aerobic exercise with anaerobic exercise.
By joining the strengthening nature of anaerobic exercise and the physiological changes mentioned in this article, it is possible to reduce pain symptoms and improve quality of life for chronic pain sufferers.
References:
Kawi, J., Lukkahatai, N., Inouye, J., Thomason, D., & Connelly, K. (2016). Effects of exercise on select biomarkers and associated outcomes in chronic pain conditions: systematic review. Biological research for nursing, 18(2), 147-159.
Naugle, K. M., Fillingim, R. B., & Riley III, J. L. (2012). A meta-analytic review of the hypoalgesic effects of exercise. The Journal of pain, 13(12), 1139-1150.
Nijs, J., Kosek, E., Van Oosterwijck, J., & Meeus, M. (2012). Dysfunctional endogenous analgesia during exercise in patients with chronic pain: to exercise or not to exercise?. Pain physician, 15(3S), ES205-ES213.
Bender, T., Nagy, G., Barna, I., Tefner, I., Kádas, É., & Géher, P. (2007). The effect of physical therapy on beta-endorphin levels. European journal of applied physiology, 100(4), 371-382.
Koltyn, K. F. (2002). Exercise-induced hypoalgesia and intensity of exercise. Sports medicine, 32(8), 477-487.
Sajedi, H., & Bas, M. (2016). The evaluation of the aerobic exercise effects on pain tolerance. Sport Science, 9, 7-11.
Naugle, K. M., & RILEY 3rd, J. L. (2014). Self-reported physical activity predicts pain inhibitory and facilitatory function. Medicine and science in sports and exercise, 46(3), 622.
Gerdle, B., Ernberg, M., Mannerkorpi, K., Larsson, B., Kosek, E., Christidis, N., & Ghafouri, B. (2016). Increased interstitial concentrations of glutamate and pyruvate in vastus lateralis of women with fibromyalgia syndrome are normalized after an exercise intervention–a case-control study. PloS one, 11(10), e0162010.
Ghafouri, N., Ghafouri, B., Fowler, C. J., Larsson, B., Turkina, M. V., Karlsson, L., & Gerdle, B. (2014). Effects of two different specific neck exercise interventions on palmitoylethanolamide and stearoylethanolamide concentrations in the interstitium of the trapezius muscle in women with chronic neck shoulder pain. Pain Medicine, 15(8), 1379-1389.







 Exercise is often recommended for many different health conditions, especially those related to the cardiovascular system, but it’s certainly not the only area where it may be extremely valuable.
Exercise is often recommended for many different health conditions, especially those related to the cardiovascular system, but it’s certainly not the only area where it may be extremely valuable.

 Caffeine has been a staple in the human diet for generations, and its social and cultural significance far exceeds that of most other psychoactive substances.
Caffeine has been a staple in the human diet for generations, and its social and cultural significance far exceeds that of most other psychoactive substances.