Multifactorial Causes of Pain – Why it’s Important to Address

Table of Contents
 Before we dive in the multifactorial causes of pain, it’s important to note that chronic pain is a complex topic that is filled with debate, and it’s even more challenging to build therapeutic programs for. There are pain scales and standardized therapy programs, but sometimes they simply are not enough to get people relief and back to their lives.
Before we dive in the multifactorial causes of pain, it’s important to note that chronic pain is a complex topic that is filled with debate, and it’s even more challenging to build therapeutic programs for. There are pain scales and standardized therapy programs, but sometimes they simply are not enough to get people relief and back to their lives.
Thus, many people are in the active search of new options to deal with their chronic issues. Yes, indeed it is a sensory impulse, just like smell and taste, but with profound emotional implications. In the long term, chronic pain affects the individual’s independence and quality of life.
If a healthy young person feels grateful after relieving short-term pain after trauma with a known recovery time, just image how important it is for people with a chronic condition who live in pain day after day for years!
In this article, we’re diving into the topic, exploring the leading causes of chronic pain and aspects you need to understand to fully appreciate the scope. You will learn why it is thought to happen, and what the doctor may be trying to communicate in a different way.
If you don’t know much about some of the thought causes of chronic pain are and why a multidisciplinary approach is recommended, then you will find your answers after reading!
What causes pain?
One of the leading authorities in chronic pain is the International Association for the study of Pain, IASP. They have recently updated the definition of pain, describing it as a sensory and emotional experience associated with tissue damage. (but of course pain doesn’t have to be associated to ANY tissue damage!)
It is inherently unpleasant and influenced by social, biological, and psychological factors. In other words, your mental state and also environmental conditions could increase or decrease your perception of pain. It usually depends on sensory impulses, but not all types of pain go through these neurons. They may also result from a malfunction in the central nervous system (1).
Accordingly, here are many causes of chronic pain. For example:
- Chronic pain associated with cancer: This type is caused by nerve compression of a growing tumor, nervous involvement, or a side effect of chemotherapy (2).
- Chronic pain after surgery or trauma: Most people have had a peculiar sensation in their surgical would during and after healing. Nerves cut in surgery and tissue damaged by trauma could trigger or worsen pain experience.
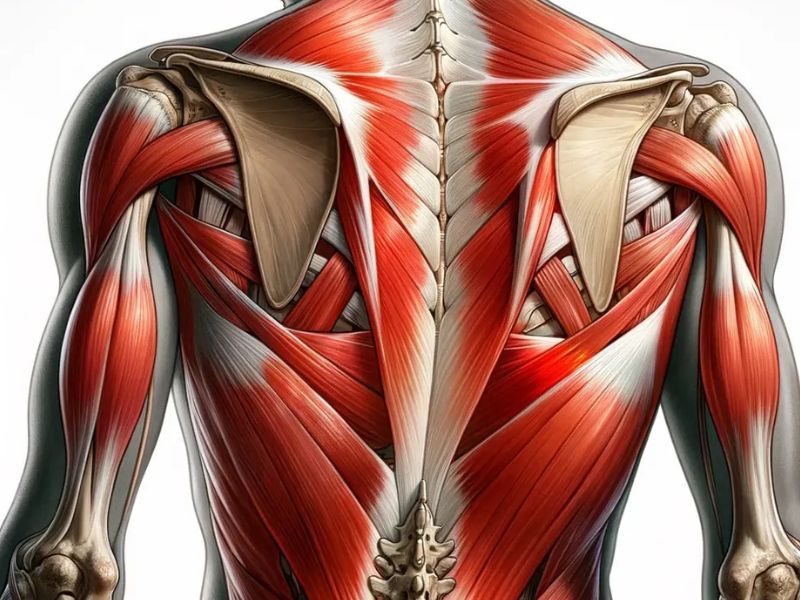
- Chronic musculoskeletal pain: This is the type of pain reported by patients with arthritis or any mechanical alteration of the musculoskeletal system. Joint pain is usually associated with inflammation, a common cause of chronic ailments (3).
- Chronic visceral pain: This pain shows up when our internal organs are inflamed for a long time or have mechanical or vascular alteration. For example, chronic pain is common in inflammatory bowel disease (4). In children, small intestinal bacterial overgrowth (SIBO) is probably one of the leading causes of chronic abdominal pain (5).
- Chronic neuropathic pain: This type of pain arises after an alteration in the nervous system. There are many pain pathways. It only takes a single lesion in one of these, and the person could end up with a relentless and very distressing type of pain. This happens in people with diabetes, and it is called diabetic neuropathy (6).
There are other contributing causes of chronic pain, and sometimes the origin is near impossible to trace. When that happens, it is often termed “primary chronic pain” and it is complicated to address.
Common ailments associated with chronic pain include:
- Migraine, glaucoma, trigeminal neuralgia, and temporomandibular joint dysfunction, leading to chronic headaches
- Carpal tunnel syndrome, muscle strains, rheumatoid arthritis, osteoarthritis, and ankylosing spondylitis, leading to chronic musculoskeletal pain
- Herpes zoster infection, multiple sclerosis, and polyneuropathies leading to chronic neurological pain
- Peptic ulcers, angina, endometriosis, and interstitial cystitis, leading to chronic abdominal or pelvic pain
What are multifactorial causes of pain?
We have reviewed several causes of chronic pain, but these individuals usually have more than one. It takes extra time to control their symptoms because it often has multiple (and often very many!) triggers. It is indeed a multifactorial pain.
Multifactorial pain is caused by several triggers at the same time. One of the best examples is low back pain. Lower back pain can be triggered by a dozen problems simultaneously. A muscle strain, chronic stress, osteoporosis, and degenerative disc disease could converge in the same person. Muscle relaxants and anti-inflammatories could reduce pain perception, but they won’t address every trigger, and the sensation still lingers despite those pharmaceutical interventions.
Essential aspects to address in multifactorial pain
Now you learned what multifactorial pain is, it will be easier to understand why some therapies may not be enough to either relieve symptoms, or keep them alleviated. In these cases, your health practitioners may explore additional options across different disciplines to get results.
Why is it important to understand pain?
As a part of chronic pain management, you’re likely to undergo a number of different evaluations to flesh out some underlying contributors to your pain.
Not fully exploring multifactorial pain could lead to either therapy failure, or a complication in the long run. This is one major reason why its important to explore the various triggers, even if it takes a good deal of time and effort to do so.
It is also essential for you to understand your specific pain experience. This way, you could find additional ways to control pain or prevent flare-ups. For example:
- Strong emotion could precipitate a flare-up in rheumatic arthritis. Ideally learning to cope with stress and eat a healthy diet would be recommended.
- Osteoporosis-related pain improves with adequate calcium consumption and exercises to strengthen back muscles and bones.
- Caffeine and alcohol could be worsening an interstitial cystitis problem.
- The main reason for joint pain could be excess bodyweight.
- Simple dietary changes like reducing carbohydrate intake and eating certain types of fermented foods could help SIBO-based discomfort.
What is the intensity of the pain?
When evaluating multifactorial pain, one of the most useful aspects is the intensity of this sensation. It is valuable information and often reflects the magnitude of the problem. Thus practitioners will try to ask patients to evaluate their own pain sensation and describe how strong it is.
The easiest way to describe pain will be using an intensity scale from 0 to 10. Zero will be no pain at all, and 10 will be excruciating pain. This is a quick way to measure the intensity of pain.
In scientific literature, pain intensity is defined as the magnitude of pain experienced by the individual. It is easier to evaluate pain intensity in adults because they have previous experience and resources to describe their condition.
Conversely, assessing pain in children is much more challenging. Besides self-report, therapists may need to evaluate their behavior and physiologic indicators.
The downside is that such indicators are usually not accurate in mild and lingering pain. In such cases, they depend on the patient’s tolerance and threshold levels (7).
Physiologic indicators and behavioral cues are also useful in adults. In this case, they are known as pain interference. It measures how pain influences the person’s physical function, mental health, and sleep patterns. Higher pain interference in chronic ailments leads to a decrease in quality of life.
Interestingly, pain intensity does not always correlate with pain interference. In other words, you can experience mild pain, but having this symptom for a very long time causes significant pain interference.
Conversely, people with acute ailments could feel more intense pain without substantial or long-term consequences in their physical function. That’s why pain interference has its own measure through the Pain Interference Subscale, included in a section of a tool known as Brief Pain Inventory (8).
What are the two types of pain scales?
As noted above, scoring pain is a fundamental step in the diagnosis. It is not always accurate and depends on the patient’s perception. However, they provide helpful insight and support doctors in assessing the extent of the problem. With no other objective measure, clinicians often depend on this type of scale and the patient’s description based on pain intensity scales.
The Brief Pain Inventory is one such tool, and there are multiple pain scales available for doctors and patients. They are all useful, and each has advantages and disadvantages. But they are broken down into two categories or types. They are unidimensional and multidimensional pain scales (9).
- Unidimensional pain scales: They are easier to use in an emergency and whenever doctors have a clearly defined and single question to ask about pain. They are easier to understand by individuals, and rating depends on their experience. Self-report is not compared with behavioral cues or the person’s physiologic response. They include the Visual Analog Scale (VAS), the Numeric Rating Scale (NRS), and the Verbal Rating/Descriptor Scale (VRS/VDS) (10).
- Visual Analog Scale: It is one of the most easy-to-understand and universal pain scales. Healthcare workers would simply draw a line and ask the person to select a point between both ends to express the intensity of the pain. One end describes no pain at all, and the other is the worst imaginable pain for them.
- Numeric Rating Scale: This scale goes one step further and divides the same line in a series of numbers from zero to ten. One of the benefits of the scale is that you can apply this tool verbally or visually. It is widely used in oral interviews with your therapist when they ask you to describe your pain on a scale from zero to ten.
- Verbal Rating Scale and Descriptor Scale: This time, instead of drawing a line or assigning numbers, the therapist asks the person to choose the word that better describes their pain. It usually includes the items “no pain”, “mild”, “moderate”, and “severe”. Similar scales could use a visual representation of faces expressing different degrees of pain with or without a written description.
- Multidimensional pain scales: We mentioned that multiple elements influence how you perceive pain. Multidimensional pain scales are created in an attempt to consider these factors. For example, they include the affective contribution, which worsens pain or helps the individual control the symptom. The person’s belief system and pain interference can also be evaluated. Multidimensional pain scales consider this symptom as the result of physiologic, psychologic, and behavioral elements. Thus, they all need to be assessed to understand pain perception. As such, they are handy in chronic conditions, especially when multiple causes of chronic pain converge in the same person.
What do multidimensional pain scales measure?
Anyone could draw a line and ask you to describe how intense your pain is. However, that won’t be enough in multifactorial pain and chronic health conditions. In these cases, multidimensional pain scales are better to assess the magnitude of the problem. They help therapists identify triggers and pain modulators, which then become potential therapeutic targets.
Scientists have developed plenty of multidimensional pain scales. Each one has its applications and benefits for a given type of chronic health condition. The best-known example is known as McGill Pain Questionnaire. This scale measures several aspects of pain using many words to describe the symptom. The person would read each word and assign a rank value. They would also assign a rank value for present pain intensity. The numbers are counted down, and the Pain Rating Index (PRI) is obtained. This tool also evaluates the exact location of the pain and how it is felt throughout time.
Other multidimensional pain scales measure additional aspects of pain. For example, the Minnesota Multiphasic Personality Inventory takes into consideration the individual’s psychology and how it affects the perception of pain. Another scale that measures a similar aspect of pain is the Pain Beliefs Questionnaire. Similarly, the Checklist for Interpersonal Pain Behavior evaluates what the person does and social considerations that modulate pain perception (9).
One of the most comprehensive multidimensional pain scales is known as the West Haven-Yale Multidimensional Pain Inventory. This scale was developed to make a complete assessment of pain in clear words and quickly. Still, it includes 12 scales, and it is divided into three parts, examining the symptom and the impact on the person’s life (11).
Most multidimensional scales are long and can be tedious to administer. Thus, abbreviated versions are made available sometimes to simplify the task. For example, there’s a short version of the McGill Pain Questionnaire. The Minnesota Multiphasic Personality Inventory also has a short version, and we have tools such as the Memorial Pain Assessment Card, a cancer-specific assessment tool that evaluates pain intensity, pain relief after therapy, and the person’s mood. It only takes a few seconds to take the test, so repeating the measure is not a burden for cancer follow-up (9,12).
Why is chronic pain management important?
Acute and chronic pain are different from each other, and pain management works differently in each case. Temporary relief with pharmaceuticals, but a comprehensive therapeutic program should also include additional considerations. Otherwise, the person may experience the adverse effects of anti-inflammatories and meds and still not get back to full functioning.
Chronic pain management is a multi-step process with many guidelines and opposing opinions. Recent research highlights the role of cognitive-behavioral therapy, exercise, and biopsychosocial rehabilitation as promising options with lower risks than opioids. Massage therapy could also offer an alternative solution, especially for chronic back pain and other musculoskeletal conditions.
Sometimes the solution requires surgical treatment, and other invasive procedures. In all cases, decisions should be made after evaluating the risks against the benefits. As opposed to acute pain relief, chronic pain management considers the multidimensional aspects of pain, standardized or coadjutant treatment, and the risks and benefits of each therapeutic option (13).
It may seem too much, and the process could be exhausting for individuals and their relatives. However, it is essential to go through this process for several reasons:
- Pain relief will improve the quality of life
- Controlling their symptoms will help them regain confidence, mobility, and independence, relieving the burden of their relatives as caregivers
- In the long-term, successful pain management may reduce costs in opioids and expensive drugs
- People are adequately educated about their condition and start contributing actively to their therapeutic program
- Newe therapeutic targets are revealed, and more options are made available
- Proper chronic pain management has a lower risk of side effects and complications
For all of the above, addressing the multiple causes of chronic pain is essential for these individuals. It is also essential to understand the basics of pain scales and other tools.
Conclusion
You can prevent annoying symptoms if you know what causes pain, but chronic conditions are much more complex. These individuals often have multifactorial causes of pain, and multiple factors contribute to their symptoms.
Something as simple as back pain could respond to osteoporosis, muscle strains, degenerative disc disease, and stress, all at the same time. If you fail to address one of these factors, you might not experience complete pain relief.
Sam Visnic
I’ve spent my life studying the fundamental aspects of human health with a focus on movement and clinical massage therapy. In a world of specialists, surgical procedures, drugs and quick fix remedies, I’m committed to finding and developing strategies that help people stuck at the “gap”. Over the last 20 years I’ve studied dozens of systems and methodologies for uncovering the root cause of aches and pains, along with postural and movement issues. Pain science, the art and science of hands-on soft tissue massage techniques, myofascial release, and coaching movement is essential in my practice. Integrating different methods but above all deciphering WHEN to use different techniques with different people and situations, along with integration of movements that people want to be able to do again is the key to long term success with my incredible track record with clients. Understanding the various elements that contribute to conditions and the power of communication and education makes my Release Muscle Therapy program separate from other hands-on therapy approaches.
Blogs You May Be Interested In
Categories
-
Deep Gluteal Pain Syndrome
-
Deltoids
-
Fallbrook
-
Foam Rolling
-
Glutes
-
Hamstrings
-
Hypnosis For Pain
-
Lats
-
Levator Scapulae
-
Lifestyle
-
Massage Therapy
-
Mobility
-
Movement and Exercise
-
Murrieta
-
Muscles
-
Nutrition
-
Obliques
-
Pain
-
Pectorals
-
Piriformis
-
Plantar Fasciitis
-
Product Review
-
Psoas
-
Quadratus Lumborum
-
Quadriceps
-
Rhomboids
-
Serratus Anterior
-
SI Joint
-
Sternocleidomastoid
-
Stretching
-
Subscapularis
-
Temecula
-
TMJ
-
Trapezius
-
Uncategorized