How To Know If Your SI Joints Are Causing Your Pain
Not too long ago, the sacroiliac joints (SIJ) were considered a primary source of lower back pain, and in particular, sciatica, however, once it was found there was no “canal that held the nerves against the joint”, the emphasis was shifted to disc herniations.
While the debate rages on, much like with spinal discs, can the sacroiliac joints be a cause of lower back pain? Well, as of recently, research is showing much more about how the SI joints can be a part of the overall pain picture.
Lets start by getting acquainted with the SI joints and how they may be cause of pain, and of course, how to address it.
What ARE The Sacroiliac Joints?
The SI joints are a part of what is referred to as the “pelvic girdle”. The main function of the pelvic girdle is to link the upper body and the lower body for movement. The pelvic girdle is made up of 3 bones and 3 joints (2 of which are the SI joints).
The bony plate at the bottom of the spine is called the sacrum, and the 2 large hip bones that are found on the left and right sides of the sacrum are called the ilia (ilium is singular). The joints at which the hip bones attach to the sacrum are the sacro-iliac joints. In the front of the pelvis, the 2 ilia are joined together by what we call the pubic joint.
The pubic joint is connected by very strong ligaments, and have opposing surfaces that keep it quite limited with regard to range of motion, but can be effected by the influence of the muscles that attach in the area, as well as hormonal changes.
The sacroiliac joints are unique in that cartilage on the sacral side is hyaline cartilage and the cartilage on the ilial side is fibrocartilage. The SI joints are L-shaped with regards to their contour, and its interesting to note that the shape of these joints vary quite dramatically from person to person, and according to Philip Greenman, DO, from side to side in the SAME person!
These joints appear to have the greatest amount of motion from age 25 to 45 (Greenman), which is very interesting, especially considering this is the age range in which back pain appears the highest, and additionally, when disc pathology is greatest.
Additionally, as both genders age, gradual changes such as fibrous adhesions and even ossification often occur, which obliterate these joints. (Grays Anatomy, Pg. 675, 1995).
2 Types of SI Joint Stability: Form and Force Closure
Generally, it is agreed there are two major stabilization systems for the SI joints, called force and form closure.
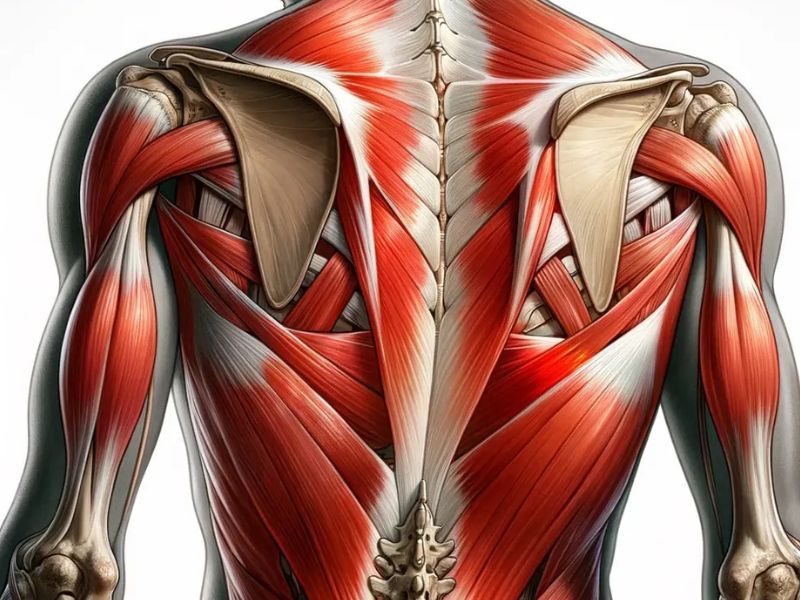
Form closure refers to the stability of the SI joints via the shape of the surfaces of the ilia on the sacrum. These surfaces are a combination of concave and convex. Force closure refers to the functioning of “slings” of muscles as well as the ligamentous support.
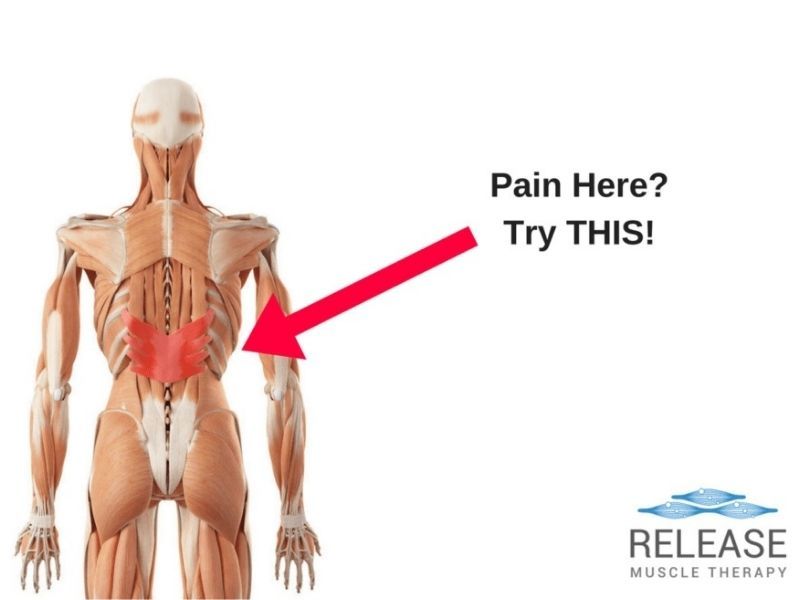
One such sling involves the glute maximus and opposite side latissmus dorsi as they merge into a super thick diamond-shaped area of connective tissue in the lower back called the thoraco-lumbar fascia.
How Do The SI Joints Cause Pain?
Frequently, SI joint dysfunction is overlooked and misdiagnosed, mostly due to the multiple effects that are seen as a result that make the overall situation appear to be multi-factorial and complicated. SI joint expert, physical therapist Richard DonTigny, has identified the following:
1. The glute medius is inhibited when held in anterior rotation
2. The ilial orgin of the gluteus maximus is separated from its sacral origin
3. The iliolumbar ligaments are loosened as the ilia approximate the vertebra
4. The long posterior ligaments will be stretched and may avulse from the PSIS
5. The ilial origin of the piriformis is separated from its sacral origin 6. If the sciatic nerve exits through the piriformis it may become painful
Yes, this is quite the complicated list! At first when the SI joint dysfunction appears, these may not all be present, but as the problem becomes chronic, some or all of them may appear and make it very difficult for the average doctor or therapist to see through to the root cause of the pain.
Depending on who the pain sufferer is seeing, and their specialty, normally accounts for what they will focus on correcting. This usually leads to failure, because only the symptoms are being addressed. At the root cause of course, is the mechanical dysfunction of the small SI joints!
How Does Sacroiliac Joint Pain Usually Show Up?
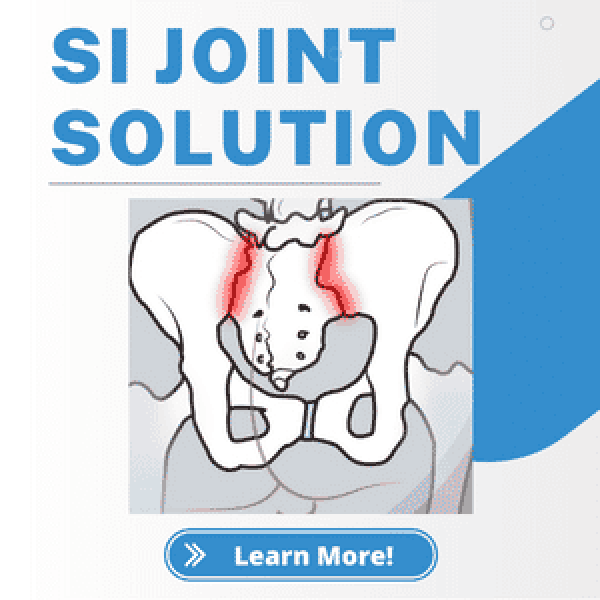
As you can see from the image, the most obvious and common area of pain related to SI joint problems is right next to the small bones that can be felt just to the sides of the lower spinal vertebrae called the posterior superior iliac spines. (PSIS for short).
Although the picture shows a relatively small region of common pain, pain patterns associated to SI joint dysfunction are highly variable due to the complex nature of nerve innervation to the joint.
The SI joints do not commonly refer pain to the lumbar spine, but that does not mean they are not frequently involved with problems in the lumbar region. It is important to keep in mind the relationship of sacroiliac joint dysfunction to disc pathology.
Disc pathology may be exacerbated by side bending and/or rotation, therefore, when the SI joints are not balanced, they will contribute to stress on vulnerable discs. It is also possible that SI joint dysfunction may actually be a factor in causing disc bulging.
Sam Visnic
I’ve spent my life studying the fundamental aspects of human health with a focus on movement and clinical massage therapy. In a world of specialists, surgical procedures, drugs and quick fix remedies, I’m committed to finding and developing strategies that help people stuck at the “gap”. Over the last 20 years I’ve studied dozens of systems and methodologies for uncovering the root cause of aches and pains, along with postural and movement issues. Pain science, the art and science of hands-on soft tissue massage techniques, myofascial release, and coaching movement is essential in my practice. Integrating different methods but above all deciphering WHEN to use different techniques with different people and situations, along with integration of movements that people want to be able to do again is the key to long term success with my incredible track record with clients. Understanding the various elements that contribute to conditions and the power of communication and education makes my Release Muscle Therapy program separate from other hands-on therapy approaches.
Blogs You May Be Interested In
Categories
-
Deep Gluteal Pain Syndrome
-
Deltoids
-
Fallbrook
-
Foam Rolling
-
Glutes
-
Hamstrings
-
Hypnosis For Pain
-
Lats
-
Levator Scapulae
-
Lifestyle
-
Massage Therapy
-
Mobility
-
Movement and Exercise
-
Murrieta
-
Muscles
-
Nutrition
-
Obliques
-
Pain
-
Pectorals
-
Piriformis
-
Plantar Fasciitis
-
Product Review
-
Psoas
-
Quadratus Lumborum
-
Quadriceps
-
Rhomboids
-
Serratus Anterior
-
SI Joint
-
Sternocleidomastoid
-
Stretching
-
Subscapularis
-
Temecula
-
TMJ
-
Trapezius
-
Uncategorized