SI Joint Myth Busting – Do Dysfunctions Really Occur?

Today we will debunk common myths surrounding sacroiliac joint dysfunction. In this article, we will provide you with evidence-based information to help you understand the truth behind SI joint dysfunction. It is important to dispel misconceptions and rely on scientific evidence when it comes to diagnosing and treating this condition.
Myth: Palpating SI Joint Movement
One common myth is that movement at the SI joint can be palpated. However, the reality is that movement at the SI joint is minimal, ranging from one to two degrees in young individuals to virtually none in the elderly. Even highly trained clinicians struggle to reach a consensus on what constitutes SI joint dysfunction. Studies have shown poor reliability for common tests used to assess SI joint movement.
Anatomical Variations and Assessment
Assessing SI joint motion manually is challenging due to anatomical variations and unreliable tests. Anatomical differences in the angle between the anterior and posterior superior iliac spines can vary significantly, making it difficult to rely solely on pelvic tilt assessment. These variations further emphasize the limitations of manual assessment in diagnosing SI joint dysfunction.
The Role of Manipulation
Manipulation of the SI joint is a common treatment approach for low back pain associated with SI joint dysfunction. However, studies have shown that manipulation does not lead to any significant changes in the position of the sacrum and ilia. The mechanism behind why some individuals experience pain relief after manipulation is not fully understood, but it is essential to consider factors other than joint repositioning.
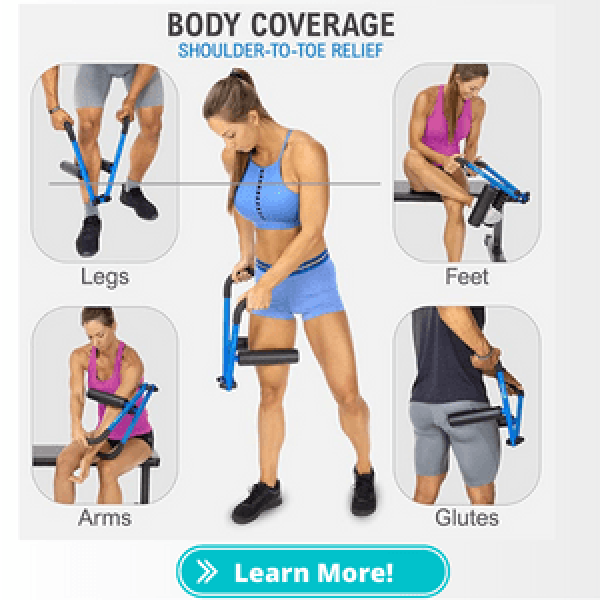
Comprehensive Approach to Low Back Pain
It is important to adopt a comprehensive approach when assessing and treating low back pain. Instead of solely focusing on the SI joint, healthcare professionals should consider other potential sources of pain, such as muscle imbalances, lumbar spine issues, or hip joint dysfunction. A thorough examination, including a detailed medical history, physical assessment, and possibly diagnostic imaging, can help identify the underlying cause of the pain more accurately.
Conclusion
By debunking the myths surrounding SI joint dysfunction and understanding the limitations of palpation and manual assessment, we can adopt a more evidence-based approach to diagnosis and treatment. It is crucial to consider the broader context of low back pain and explore multiple potential sources of pain. By doing so, we can provide more accurate diagnoses and implement appropriate management strategies for pain sufferers.
Sam Visnic
I’ve spent my life studying the fundamental aspects of human health with a focus on movement and clinical massage therapy. In a world of specialists, surgical procedures, drugs and quick fix remedies, I’m committed to finding and developing strategies that help people stuck at the “gap”. Over the last 20 years I’ve studied dozens of systems and methodologies for uncovering the root cause of aches and pains, along with postural and movement issues. Pain science, the art and science of hands-on soft tissue massage techniques, myofascial release, and coaching movement is essential in my practice. Integrating different methods but above all deciphering WHEN to use different techniques with different people and situations, along with integration of movements that people want to be able to do again is the key to long term success with my incredible track record with clients. Understanding the various elements that contribute to conditions and the power of communication and education makes my Release Muscle Therapy program separate from other hands-on therapy approaches.
Blogs You May Be Interested In
Categories
-
Deep Gluteal Pain Syndrome
-
Deltoids
-
Fallbrook
-
Foam Rolling
-
Glutes
-
Hamstrings
-
Hypnosis For Pain
-
Lats
-
Levator Scapulae
-
Lifestyle
-
Massage Therapy
-
Mobility
-
Movement and Exercise
-
Murrieta
-
Muscles
-
Nutrition
-
Obliques
-
Pain
-
Pectorals
-
Piriformis
-
Plantar Fasciitis
-
Product Review
-
Psoas
-
Quadratus Lumborum
-
Quadriceps
-
Rhomboids
-
Serratus Anterior
-
SI Joint
-
Sternocleidomastoid
-
Stretching
-
Subscapularis
-
Temecula
-
TMJ
-
Trapezius
-
Uncategorized