Pudendal Nerve Entrapment | How To Identify And Self Help

Table of Contents
- - What is the pudendal nerve, and where is it located?
- - How does the pudendal nerve get entrapped? What are the causes?
- - What are the symptoms of pudendal nerve entrapment?
- - How is it diagnosed?
- - Differential diagnoses
- - How is pudendal neuralgia treated?
- - What conservative measures are used?
- - References:
In some cases, even the best specialists have no final answer. Meanwhile, many patients suffer from symptoms with no idea about what to do.
One such problem is pudendal nerve entrapment. It tends to be a condition that’s difficult to diagnose. However, there are ways to identify the problem with proper attention to the signs and symptoms. Once the problem is located, we can alleviate the symptoms with something as simple as lifestyle modifications.
Information is key, especially concerning the identification of the problem. So, let’s take a brief look at the issue and how to achieve a bit of self-help. As we move on, remember it’s important to discuss what you read with your healthcare provider before making any decision on your health.

What is the pudendal nerve, and where is it located?
The pudendal nerve is a branch of the sacral spinal nerves, a nerve bundle found in the lower portion of the spine, between S2 and S4. It runs around the pelvis from the spine to the genitals.
On its way, it leaves different branches and picks up sensations from the skin and other pelvic structures. Such sensory recollection includes your external genitalia and anus.
Thus, the pudendal nerve is essential during intercourse to feel sexually stimulated. Damage to this nerve can have profound implications on sexual enjoyment. As such, it is definitely a health issue with plenty of social and psychological implications.
Before it goes through the pudendal canal (Alcock canal) and reaches the genitals, the pudendal nerve passes through the deep gluteal area. Here, it comes into contact with ligaments such as the sacrospinous and muscles such as the piriformis (1).
How does the pudendal nerve get entrapped? What are the causes?
The pudendal nerve may cause pain for various reasons. For example, endometriosis can irritate the pudendal nerve and trigger the symptoms.
But a frequent cause of pain will be nerve entrapment. It occurs when other structures place mechanical pressure on the nerve.
Where it gets entrapped
Since the pudendal nerve runs adjacent to various muscles and through bones and canals, it can get impinged in many areas.
For instance (2):
- Below the piriformis muscle, causing entrapment syndrome type I.
- Between the sacrotuberous and sacrospinous ligaments, causing an entrapment syndrome type II.
- In the Alcock canal, causing an entrapment syndrome type III.
- In its terminal portion, it causes an entrapment syndrome type IV.
Depending on the location, pudendal entrapment can trigger specific signs and symptoms a therapist can identify.
Causes of pudendal nerve entrapment
The primary causes of pudendal nerve compression include (2):
- Following surgery on the pelvis, especially when surgeons leave a mesh in place.
- As a result of stretching in a vaginal delivery.
- In response to direct trauma to the buttocks or lower back.
- In case of excessive cycling on an inadequate seat. This triggers microtrauma and fibrosis in the Alcock canal.
- In people who remain seated for very long periods.
- Occasionally, chronic constipation may also contribute to the problem.
What are the symptoms of pudendal nerve entrapment?
When a compression of the pudendal nerve occurs, it causes symptoms in the genitals and pelvic floor. For example (3,4):
- Burning pain in the perineum, rectum, and/or genitals.
- Numbness in the perineum, rectum, and/or genitals.
- Pain or discomfort increases when sitting. It improves when standing or sitting on a toilet.
- Pain can be triggered or worsened after bowel movements
- Pain is predominant on one side
- Pain improves when lying down at night. Thus, it does not awaken the patient from their sleep.
- A sensation of urgency to urinate
- Foreign body sensation in the anus, urethra, or vagina
- Painful urination (dysuria)
- Painful ejaculation in men
- Other types of sexual dysfunction, such as dyspareunia, male erectile problems, and arousal dysfunction
- Fecal incontinence or constipation
- As with other types of chronic neuropathic pain, it can also lead to anxiety, depression, and similar issues.
About the symptoms of pudendal entrapment, specialists from Rochester University mention that “the main symptom is pain with sitting. You feel great in the AM until you sit for coffee, or drive to work. You get better with lying down”.
Thus, every patient is different and you’re unlikely to experience all symptoms at once. But the one that’s usually there is pain with sitting.
How is it diagnosed?
The diagnosis of pudendal nerve damage is often challenging. Due to its complexity, it should be guided by a doctor, physical therapist, or another specialist. Diagnosing pudendal entrapment involves different phases which contribute to the process (2,3):
1. Considering the symptoms
Initially, your healthcare provider will evaluate the symptoms of pudendal nerve entrapment. Physical examination may also aid in the diagnosis.
Depending on the signs and symptoms, your therapist can guess the site of entrapment.
For example, an impingement below the piriformis causes spasms of the piriformis muscle. An entrapment in the pudendal canal causes spasms in the obturator internus muscle. A therapist can identify these signs accurately on the physical exam.
2. Nerve blocks
A doctor may also use nerve blocks to diagnose pudendal nerve entrapment. It involves injecting anesthesia into the portion of the pudendal nerve that passes through the deep gluteal space.
3. Imaging tests
In addition, some specific tests may help. For example, an ultrasound may show a flattened nerve or liquid retention (5). MRI is also helpful in identifying the exact location of the nerve entrapment (6).
4. Ruling out other causes
Pudendal nerve entrapment symptoms are similar to numerous chronic pain syndromes and other ailments. It is one of the reasons why it is difficult to diagnose. It often requires ruling out other health problems that trigger persistent pelvic pain. For example, through a vaginal or rectal exam.
In some cases, your therapist or doctor will make recommendations to reduce overlapping symptoms of other pain contributors. Pudendal nerve entrapment syndromes are easier to diagnose after ruling out similar diagnoses.
Differential diagnoses
What ailments should we rule out?
For example, pain triggered by sitting is also frequent in deep gluteal pain syndrome. Similarly, prostatitis can also trigger pelvic floor pain. It is also essential to rule out some sexually transmitted diseases. Two differential diagnoses worth mentioning include (7):
Hamstring tendinopathy
It also causes pain aggravated by sitting. In this case, however, patients usually feel a boggy mass in the gluteal area. A simple physical exam can help your therapist determine if you have hamstring tendinopathy.
Piriformis syndrome
It causes buttock or pelvic pain and is also associated with nerve impingement. However, in this case, the affected nerve is the sciatic nerve. Since the piriformis is also in contact with the pudendal nerve, you can sometimes have both nerves affected simultaneously.
How is pudendal neuralgia treated?
Pudendal neuralgia may require surgical treatment (pudendal nerve decompression). However, most others respond to conservative measures and lifestyle changes.
One of the most important recommendations is to avoid positions and activities that trigger pain. There are also physical therapy exercises designed for the pelvic floor. By relaxing these muscles, it is possible to reduce pain in some patients.
Of course, we can also use oral medications, such as analgesics, muscle relaxants, and anticonvulsants.
It is essential to highlight that not all patients will respond the same way. Depending on the site of entrapment and the cause, you may respond to one treatment protocol and not the other (2).
When conservative treatment fails, surgical decompression is a suitable option. Even so, minimal access surgical techniques may solve the problem. In a study published in the Journal of Neurosurgery, the investigators found that 87% of cases improved with a type of surgery that does not require too much cutting through (3).
What conservative measures are used?
As a massage therapist specializing in massage therapy, muscle release, and pain science, my main focus is conservative treatment. Do you know the conservative approaches available for pudendal entrapment?
Here’s what I typically recommend (2):
Physical therapy
Depending on the compression zone, pelvic floor physical therapy can be quite helpful. For example:
- When the pain comes from a muscle spasm, physical therapy can relax the muscle. The type of physical therapy available for pelvic floor muscles involves neuromuscular massage therapy. This technique is designed to detect and release muscle tension where the pudendal nerve runs.
- Your therapist can offer traditional physical therapy combined with transcutaneous electrical nerve stimulation (TENS). This technique is not expensive and is associated with better results.
Oral therapy
As mentioned above, doctors may recommend analgesics, muscle relaxants, and anticonvulsants.
- Analgesics reduce the sensation of pain, as we all know.
- Muscle relaxants improve pain when muscle tension is affecting the pudendal nerve. They may not work in other causes of compression.
- Anticonvulsants reduce the constant firing of the pudendal nerve. That’s how they improve pain symptoms.
Pudendal nerve blocks
These injections come in handy to complete the diagnosis. Pudendal nerve pain subsides for a few minutes or hours.
However, some patients experience a more extensive pain relief. In these patients, doctors can use a pudendal nerve block to reduce nerve irritation and improve the quality of life.
Lifestyle changes
In addition to medical treatment and physical therapy, there is much you can do on a self-help approach. The following recommendations tend to work and reduce pelvic pain in pudendal neuropathy (2,7):
- If you are a cyclist, make sure you have a properly padded seat.
- Discontinue any sporting activity in case it triggers pain.
- Avoid rowing, skiing, jogging, and other exercises that require constant hip flexion.
- If you have an office job, alternate sitting and standing periods.
- Invest in a workstation you can use while standing, such as a standing desk.
- Weight loss can sometimes help the treatment. Try to maintain or achieve a healthy weight.
- Chronic perineal pain can cause sexual dysfunction with serious psychological implications. Seek counseling if you experience frustration, anxiety, depression, and similar problems.
These recommendations may not seem a big deal. However, 20-30% of patients get better just by applying them. Another percentage improves with therapy, medical treatment, and following these recommendations. Decompression surgery is recommended only in severe cases or those that do not respond to other modalities.
Still, all we considered in this article does not substitute professional advice from a licensed therapist or doctor. It is important to consult with your healthcare provider and make a treatment plan together based on a personalized treatment approach. Doing so will get you much closer to relieving pain and improving your quality of life.
References:
- Kinter, K. J., & Newton, B. W. (2020). Anatomy, abdomen and pelvis, pudendal nerve.
- Kaur, J., & Singh, P. (2019). Pudendal nerve entrapment syndrome.
- Filler, A. G. (2009). Diagnosis and treatment of pudendal nerve entrapment syndrome subtypes: imaging, injections, and minimal access surgery. Neurosurgical focus, 26(2), E9.
- Labat, J. J., Riant, T., Robert, R., Amarenco, G., Lefaucheur, J. P., & Rigaud, J. (2008). Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurourology and Urodynamics: Official Journal of the International Continence Society, 27(4), 306-310.
- Mollo, M., Bautrant, E., Rossi-Seignert, A. K., Collet, S., Boyer, R., & Thiers-Bautrant, D. (2009). Evaluation of diagnostic accuracy of colour duplex scanning, compared to electroneuromyography, diagnostic score and surgical outcomes, in pudendal neuralgia by entrapment: a prospective study on 96 patients. Pain, 142(1-2), 159-163.
- Wadhwa, V., Hamid, A. S., Kumar, Y., Scott, K. M., & Chhabra, A. (2017). Pudendal nerve and branch neuropathy: magnetic resonance neurography evaluation. Acta Radiologica, 58(6), 726-733.
- Castellanos, M. E., de Souza, K., & Hibner, M. (2021). Pudendal Neuralgia. Management of Chronic Pelvic Pain: A Practical Manual, 156.
Sam Visnic
I’ve spent my life studying the fundamental aspects of human health with a focus on movement and clinical massage therapy. In a world of specialists, surgical procedures, drugs and quick fix remedies, I’m committed to finding and developing strategies that help people stuck at the “gap”. Over the last 20 years I’ve studied dozens of systems and methodologies for uncovering the root cause of aches and pains, along with postural and movement issues. Pain science, the art and science of hands-on soft tissue massage techniques, myofascial release, and coaching movement is essential in my practice. Integrating different methods but above all deciphering WHEN to use different techniques with different people and situations, along with integration of movements that people want to be able to do again is the key to long term success with my incredible track record with clients. Understanding the various elements that contribute to conditions and the power of communication and education makes my Release Muscle Therapy program separate from other hands-on therapy approaches.
Blogs You May Be Interested In
Categories
-
Deep Gluteal Pain Syndrome
-
Deltoids
-
Fallbrook
-
Foam Rolling
-
Glutes
-
Hamstrings
-
Hypnosis For Pain
-
Lats
-
Levator Scapulae
-
Lifestyle
-
Massage Therapy
-
Mobility
-
Movement and Exercise
-
Murrieta
-
Muscles
-
Nutrition
-
Obliques
-
Pain
-
Pectorals
-
Piriformis
-
Plantar Fasciitis
-
Product Review
-
Psoas
-
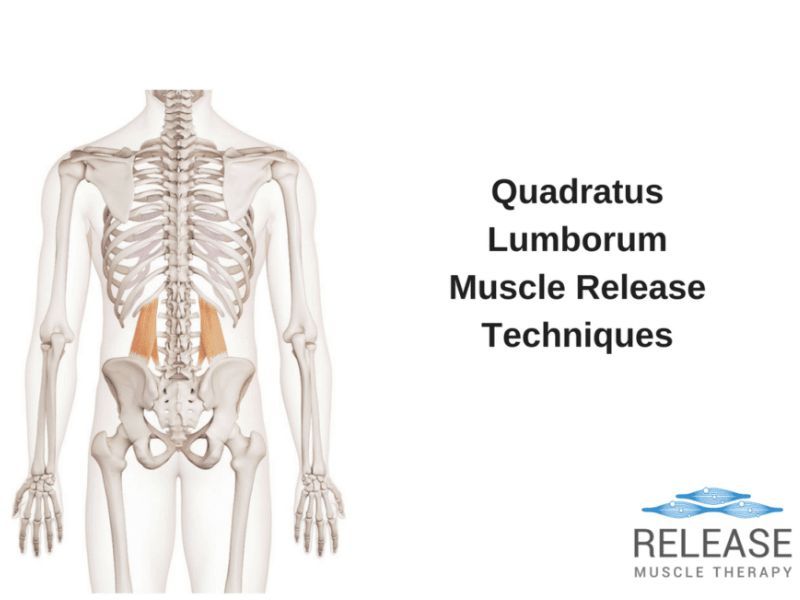
Quadratus Lumborum
-
Quadriceps
-
Rhomboids
-
Serratus Anterior
-
SI Joint
-
Sternocleidomastoid
-
Stretching
-
Subscapularis
-
Temecula
-
TMJ
-
Trapezius
-
Uncategorized