Managing Deep Gluteal Pain: Guide to Piriformis Syndrome and Buttock Pain

Table of Contents
- - What is Deep Gluteal Pain?
- - Causes of Deep Gluteal Pain
- - Symptoms of Deep Gluteal Pain
- - Diagnosis
- - Discriminating signs and symptoms
- - Physical examination basics
- - Deep gluteal pain testing
- - Diagnostic imaging
- - Deep Gluteal Pain vs. Other Conditions
- - Treatment Options
- - How to Treat Deep Gluteal Pain at Home
- - FAQs
- - Can deep gluteal pain be chronic?
- - How does deep gluteal pain affect leg abduction?
- - When should I consider surgery for deep gluteal pain?
- - How long does it typically take to recover from deep gluteal pain?
- - Can deep gluteal pain be a sign of a more serious underlying condition?
- - Conclusion
- - References:
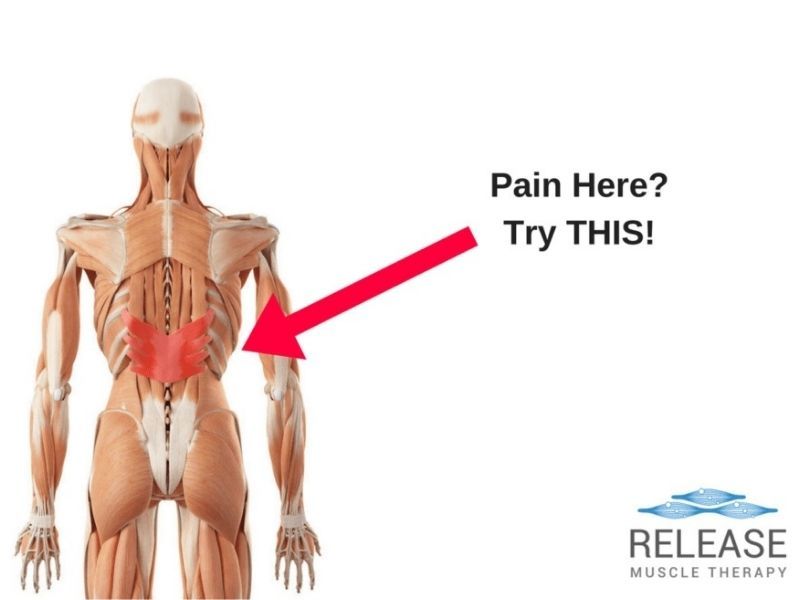
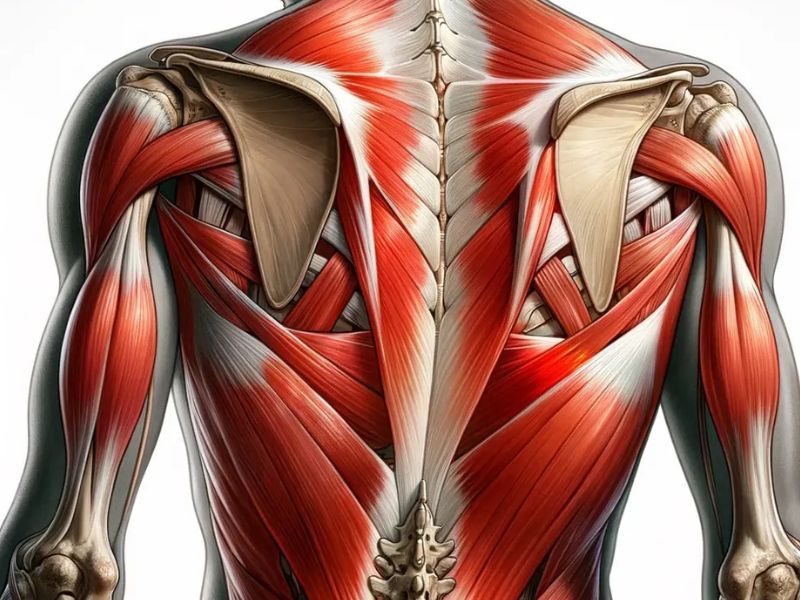
Buttock complexity is often underestimated. However, they are an intricate web of overlapping muscle layers, nerves, and blood vessels.
What happens when it goes awry? What is deep gluteal pain? Where does it come from?
As the name suggests, deep gluteal pain originates in the intermediate or deep muscle layers. This stealthy intruder often connects to a sciatic nerve entrapment syndrome, such as the notorious sciatica.
Just imagine not being able to sit comfortably for more than 15 minutes. That’s an everyday problem for some people, even athletes (1). So, the importance of treating deep gluteal syndrome becomes evident after experiencing the symptoms.
Deep gluteal pain is not a minor inconvenience. It can become a disabling problem in older adults and a performance killer in young people.
That is why we devoted this hub page to shine a spotlight on this perplexing ailment.
[lwptoc]
What is Deep Gluteal Pain?

What is the actual definition of deep gluteal pain?
It’s a sensation of numbness or a distinct pain in the buttocks. But what makes deep gluteal pain different vs regular gluteal pain? It is the nerve entanglement factor.
It often causes radiation pain along the distribution of the sciatic nerve anatomy (sciatic nerve pain). Deep gluteal pain is considered a sciatic nerve disorder, unlike regular buttock pain. It is untethered from disc issues and features sciatic nerve entrapment in the deep gluteal space (2).
As noted, it is much more complex and goes beyond simple, transient pain. It usually comes with psychosocial consequences, movement limitations, and a plummet in your quality of life.
Causes of Deep Gluteal Pain
The deep gluteal space is complex. Each component can be a pain trigger. The potential cause can be a muscle, tendon, or nerve. Each can generate pain due to different processes. For instance:
Entrapment neuropathy
It features pinching or pressure upon a nerve, which triggers pain. It is one of the most common causes of deep gluteal pain. One example is the ever-troublesome piriformis muscle, which often causes sciatic nerve entrapment (3).
Lesions and fractures
Inflammation is a common trigger of deep gluteal pain. It can originate from an injury or fracture. For example, repetitive movements can cause micro-tears in the muscle tissue. It swells and puts pressure on nerve structures. This cause of deep gluteal pain is common in sports injuries in and around the gluteal triangle region (4).
Enthesopathy and tendinopathy
Tendon disorders such as tendinitis can cause deep gluteal pain. There is also connective tissue connecting tendons and bones (entheses). These ailments can also trigger deep gluteal syndrome. A few potential culprits here include the quadratus femoris muscle, piriformis muscle, and gluteus medius (5).
Uncommon causes
Can ovulation cause deep gluteal pain? Yes, some patients develop deep gluteal pain during pregnancy or ovulation.
However, this is a type of referred pain. The trigger can be intra-abdominal or intra-pelvic inflammatory processes. Endometriosis, irritable bowel syndrome, and even inguinal hernia may also cause these symptoms (2).
Trigger points in the gluteals may also be a contributing factor in some cases.
The triggers are outside the deep gluteal space, which is why some professionals do not include them in the deep gluteal syndrome. Also, it does not feature sciatic nerve compression. Therefore, seeking professional help is essential to rule out a differential diagnosis and alleviate your symptoms.
Symptoms of Deep Gluteal Pain
Deep gluteal pain symptoms may include (2,6):
- Buttock pain or numbness
- Pain radiated to the knee (sciatic nerve symptoms)
- Pain triggered by prolonged sitting
- Walking in short strides for pain avoidance
- Sensory changes and pain upon palpation
- Disturbed sleep due to severe pain at night
- Locking or clicking sounds on the hip joint
- Limping after prolonged sitting
These symptoms of deep gluteal pain do not follow a set script. For instance, nerve entrapment can be vague and hard to pinpoint. Symptoms may come and go and change location, varying in intensity depending on the cause.
However, in almost all cases, deep gluteal pain features nerve entrapment, Thus, it includes a combination of radiating sciatic pain and limping. Depending on the cause, different signs and symptoms may add up. For example:
- Hamstring tendinopathy could make you feel a “boggy mass” in your hips with weight-bearing activities or after sitting.
- Gluteal tendinopathy gives you night pain when lying on the affected side.
- In pudendal nerve entrapment, using a seat or riding a bicycle increases the pain, but sitting on a toilet might bring some relief.
It’s a complex puzzle, and each piece matters. So, communicating your symptoms can make a difference in the diagnostic process.
Diagnosis
The symptoms of deep gluteal pain are often cryptic. However, your therapist will sort them out and perform a few physical examination maneuvers and tests to reveal the diagnosis.
What exams and maneuvers work to diagnose deep gluteal pain?
Discriminating signs and symptoms
An understanding of deep gluteal space is fundamental. It will help your therapist rule out similar-sounding culprits.
You may drop a big hint that points directly to a diagnosis. In other cases, a workup will help rule out different possibilities and reveal the source of pain.
The most common symptoms are pain in the buttocks and retrotrochanteric regions. This sciatic pain often radiates to the posterior thigh but may also radiate to the perineum or groin (6).
Physical examination basics
Physical therapists may also assess whether hip flexion or rotation worsens the pain and whether it flares up during physical activity or extended sitting.
With a physical examination, paresthesia, numbness, trigger points, and tender areas can also be detected. Different landmarks can guide the way of palpation, such as the greater trochanter, ischial tuberosity, and iliac crest (2).
When signs and symptoms are unclear, a thorough physical evaluation should be performed. It may include the spine, hip, pelvis, and abdomen examination. As tiring as it may seem, it is a crucial piece of the puzzle.
Deep gluteal pain testing
You may need to undergo a series of passive and active movement tests with your provider. Remember these are important to get to the bottom of things, and you should communicate your sensations throughout.
Special tests include internal rotation of the hip, the flexion test, and the seated piriformis stretch test, which can help diagnose piriformis syndrome. The piriformis muscle provocation test is also beneficial to diagnose sciatic nerve entrapment (7).
Diagnostic imaging
Imaging tests may confirm the diagnosis or rule out other potential causes. For example, X-rays can spot bone pathologies, but they are not the most commonly used.
Nerve conduction studies help detect sciatic nerve entrapment. However, an MRI is the most convenient to rule out specific underlying contributors and assist with diagnosing the root cause of deep gluteal pain.
MRI unveils abnormal fibrous bands, atrophy, muscle hypertrophy, and muscle or tendon tears. Magnetic resonance neurography may even show nerve trace abnormalities in the deep gluteal space.
In mechanical neuropathies, MRI can identify the presence of fascicular edema and perifascicular fat abnormalities. Note that MRI will not always serve to confirm a diagnosis. But even when magnetic resonance neurography and similar tools do not confirm a diagnosis, it is always valuable to rule out other pathologies (8).
Ultrasound can also play a crucial role, adding real-time evaluations to the diagnostic arsenal. Doctors may carry out tests such as internal and external hip rotation to evaluate how it looks from deep within. Ultrasound can also guide palpation and identify structures likely to be a source of pain, such as nerves, tendons, and gluteal muscles (9).
Deep Gluteal Pain vs. Other Conditions
Deep gluteal pain has many differential diagnoses. In other words, different conditions can masquerade the signs and symptoms listed above. But there were also terminology changes over time, which is often a source of confusion.
So, when you read about other conditions with the same list of signs and symptoms, remember that deep gluteal pain syndrome is a relatively new term. It started to be used in the literature as new pathologies were added as potential causes of the same syndrome. The new term encompasses all of them.
The best way to explain this is through a few examples (6):
Piriformis syndrome
It is also known as fat wallet syndrome or walled sciatica. The term has been around since the 1930s. It was formally adopted as medical terminology in the literature by 1947. But what’s the difference between piriformis syndrome vs deep gluteal pain?
Today, the term is still used despite the tendency to change it to deep gluteal syndrome. It’s because the term can be misleading. It implies that the piriformis muscle alone is to blame for the symptoms we just described. As a new term, deep gluteal syndrome casts a wider net. It also encompasses new entities health professionals should consider.
Proximal hamstring tendinopathy
Hamstring deep gluteal pain has undergone a name evolution, too. It occurs due to repetitive loading and strain over the hamstring and its tendon.
Repetitive motion causes micro-tears, inflammation, thickening of the tendon, and compression of the underlying nerve (sciatic nerve entrapment). Rupture of the tendon may also occur.
This entity can be a cause of deep gluteal pain. Thus, similar to the piriformis syndrome, it is encompassed in the deep gluteal syndrome.
Trochanteric bursitis
This entity features inflammation in the bursa of the greater femoral trochanter. Thus, trochanteric bursitis can trigger deep gluteal pain, but hip pain is the most common symptom.
People with trochanteric bursitis usually present with pain on the outside of the hip and posterior thigh. It is one of the differential diagnoses to consider in a case of buttock pain.
Treatment Options
Treating deep gluteal pain may require different modalities and strategies. The main highlights are medication and physical therapy. Encouraging relative rest and adjustments in certain activities and habits is also essential.
Medications
Oral analgesics are often the first-line treatment. These reduce inflammation and help manage pain.
These medications can be used along with muscle relaxants when the source of the problem is muscle tension. Oral medication is often replaced with intramuscular or intravenous therapy in more severe cases (2,7).
Physical therapy
Depending on the pain trigger, there are different sets of exercises for deep gluteal pain relief. Some require the assistance of a therapist. You can do others at home.
Consistency and following instructions for the allotted time are the key. Follow the instructions to the letter and ask your physical therapist before trying something new (7).
Most professionals will recommend physical therapy rehabilitation for a minimum of six weeks. It consists of exercises to strengthen hip mechanics, tendons, and muscles involved in lower extremity movement.
Some exercises are designed to mobilize sciatic nerve entrapment in the gluteal region. This sciatic nerve glide improves flexibility and stabilizes your symptoms (2).
Massage therapy
The main massage for deep gluteal pain is neuromuscular massage therapy. It is also referred to as myofascial release or trigger point therapy.
This technique consists of applying pressure for 30 seconds to two minutes with the appropriate intensity on the right trigger point. Therefore, this technique should be administered by a professional (10).
You can also benefit from self-massage at home with foam rollers or replacing them with a tennis ball (2).
Experimental and complementary treatment
Some tough cases can improve with manual therapy, trigger point injections, and acupuncture. However, there is not enough evidence to use these methods systematically.
There are also reports with results with botulism toxin injections in the piriformis muscle. However, this approach can cause complications, such as fibrosis of the sciatic nerve (2).
Surgical treatment
Sometimes, surgery is the only resource to achieve pain relief. There are different surgical approaches, such as open decompression of the sciatic nerve or endoscopic procedures. For severe cases, this can be a game-changer in hamstring or piriformis muscle syndrome, and traumatic causes of deep gluteal syndrome (7).
How to Treat Deep Gluteal Pain at Home
How to treat gluteal pain at home? There are many options out there besides traditional medical treatment. They do not replace medical therapy but may help you find comfort at home. Here’s a summary of the most effective home remedies, stretches, and recommendations (2).
Activity modifications
Pay attention to any activity modifications proposed by your doctor and physical therapist. Depending on the source of the pain, you may need to make some changes.
For example, in hamstring tendinopathy, you should avoid bending activities, especially deadlift exercises. Also, avoid stretching the hamstrings unless directly recommended by your therapist.
In all cases of sciatic nerve entrapment, alternating periods of sitting and standing can make a lot for you. Likewise, doctors and therapists may recommend drivers to move the seat closer to the steering wheel. If you’re a runner, you may need to reduce your stride length.
Additional recommendations
Further changes include shedding excess weight and quitting smoking. Also, anti-inflammatory foods can be suitable home remedies for deep gluteal pain, such as turmeric and omega 3.
Ice and low temperatures can also improve pain temporarily. However, do not apply ice directly to the skin. Use a cloth to keep your skin apart, and use ice therapy for five minutes to avoid ice burns.
Stretches and exercises
There’s a range of deep gluteal pain stretches to try at home. The recommended set of exercises is not the same for all patients. Therefore, always consult your therapist before embarking on any new routine.
Here are a few examples of exercise for deep gluteal pain:
- Some patients with piriformis syndrome may benefit from a piriformis muscle and glute stretch with a foam roller. To perform this exercise, lie on the floor with your buttocks resting on the foam roller. With the knees bent, move forward and backward to stretch the gluteus muscles.
- Another exercise is the glute stretch lying. Lie on the floor bending your knees at 90°. Cross one ankle with the opposite knee. Push until you feel a little stretch. Repeat on the other side.
- Sitting exercises can also be done, such as the piriformis muscle stretch sitting. It is very similar to glute stretch lying, but instead of lying on your back, you will sit on a chair. After crossing your ankle with the knee on each side, lean forward until you feel the stretch in your buttocks.
FAQs
Can deep gluteal pain be chronic?
Yes. Chronic deep gluteal pain can develop when a long-standing ailment is causing the symptoms. Some cases of recurrent or refractory pain can reach a chronic state.
That is why doctors leave surgery as a last resort, but there are still patients who are not candidates. They should seek supportive treatment rather than a curative approach and may still experience chronic pain.
How does deep gluteal pain affect leg abduction?
Deep gluteal pain with leg abduction can be a sign of piriformis muscle involvement. This movement can be used in the physical examination as one of the maneuvers to identify the source of the pain. It is a sign of inflammation of the piriformis muscle or sciatic nerve irritation.
When should I consider surgery for deep gluteal pain?
Surgery is the last treatment option for patients who do not respond to medical treatment and physical therapy. In most cases, conservative treatment is sufficient to improve lifestyle and, in many cases, solve the underlying problem.
How long does it typically take to recover from deep gluteal pain?
Recovery may take 6 to 12 weeks, depending on the trigger and the severity of the complaint. During this time you should follow the instructions of your doctor or therapist to speed up the results.
Can deep gluteal pain be a sign of a more serious underlying condition?
Other problems outside the deep gluteal space can also trigger these symptoms. For example, hip joint osteoarthritis may cause referred pain in the buttocks. Something similar can also occur in femoral neck fractures and other serious injuries outside the deep gluteal region.
Conclusion
Navigating the intricacies of deep gluteal syndrome can feel quite challenging. But let’s have a deep gluteal pain summary.
In short, deep gluteal pain syndrome is a localized pain in the buttocks. It often radiates due to sciatic nerve entrapment (sciatic pain). It was known as piriformis syndrome for many years, but the term is being updated to encompass other pathologies of the deep gluteal space.
The pain results from abnormalities in the muscles such as the piriformis muscle, tendons such as the hamstring tendon, and other structures of the deep gluteal space. It features an umbrella of conditions that demand thorough evaluation.
So, if you are grappling with deep gluteal pain, ask your healthcare provider and seek professional help before it becomes unbearable. After a physical examination and some tests, a diagnosis and accurate treatment will be possible.
Do not hesitate to come to a professional for deep gluteal pain. Most patients find relief through conservative treatment and physical therapy, making a profound difference in their quality of life.
References:
- Podschun, L., Hanney, W. J., Kolber, M. J., Garcia, A., & Rothschild, C. E. (2013). Differential diagnosis of deep gluteal pain in a female runner with pelvic involvement: a case report. International journal of sports physical therapy, 8(4), 462.
- Hu, Y. W. E., Ho, G. W., & Tortland, P. D. (2021). Deep gluteal syndrome: a pain in the buttock. Current Sports Medicine Reports, 20(6), 279-285.
- McCrory, P., & Bell, S. (1999). Nerve entrapment syndromes as a cause of pain in the hip, groin, and buttock. Sports Medicine, 27, 261-274.
- Franklyn-Miller, A., Falvey, E., & McCrory, P. (2009). The gluteal triangle: a clinical patho-anatomical approach to the diagnosis of gluteal pain in athletes. British journal of sports medicine, 43(6), 460-466.
- Ohm-Pedersen, K. (2018). Gluteal Tendinopathy. Clinical Practice Guidelines, 357.
- Carro, L. P., Hernando, M. F., Cerezal, L., Navarro, I. S., Fernandez, A. A., & Castillo, A. O. (2016). Deep gluteal space problems: piriformis syndrome, ischiofemoral impingement, and sciatic nerve release. Muscles, ligaments and tendons journal, 6(3), 384.
- Martin, H. D., & Gómez-Hoyos, J. (2019). Deep gluteal syndrome. Posterior Hip Disorders: Clinical Evaluation and Management, 167-187.
- Hernando, M. F., Cerezal, L., Pérez-Carro, L., Abascal, F., & Canga, A. (2015). Deep gluteal syndrome: anatomy, imaging, and management of sciatic nerve entrapments in the subgluteal space. Skeletal radiology, 44(7), 919-934.
- Chang, K. V., Wu, W. T., Lew, H. L., & Özçakar, L. (2018). Ultrasound imaging and guided injection for the lateral and posterior hip. American Journal of Physical Medicine & Rehabilitation, 97(4), 285-291.
- Awan, W. A., & Babur, M. N. (2011). Effectiveness of deep friction massage & stretching exercises in piriformis syndrome. IJCRB, 3(03), 378-383.
Sam Visnic
I’ve spent my life studying the fundamental aspects of human health with a focus on movement and clinical massage therapy. In a world of specialists, surgical procedures, drugs and quick fix remedies, I’m committed to finding and developing strategies that help people stuck at the “gap”. Over the last 20 years I’ve studied dozens of systems and methodologies for uncovering the root cause of aches and pains, along with postural and movement issues. Pain science, the art and science of hands-on soft tissue massage techniques, myofascial release, and coaching movement is essential in my practice. Integrating different methods but above all deciphering WHEN to use different techniques with different people and situations, along with integration of movements that people want to be able to do again is the key to long term success with my incredible track record with clients. Understanding the various elements that contribute to conditions and the power of communication and education makes my Release Muscle Therapy program separate from other hands-on therapy approaches.
Blogs You May Be Interested In
Categories
-
Deep Gluteal Pain Syndrome
-
Deltoids
-
Fallbrook
-
Foam Rolling
-
Glutes
-
Hamstrings
-
Hypnosis For Pain
-
Lats
-
Levator Scapulae
-
Lifestyle
-
Massage Therapy
-
Mobility
-
Movement and Exercise
-
Murrieta
-
Muscles
-
Nutrition
-
Obliques
-
Pain
-
Pectorals
-
Piriformis
-
Plantar Fasciitis
-
Product Review
-
Psoas
-
Quadratus Lumborum
-
Quadriceps
-
Rhomboids
-
Serratus Anterior
-
SI Joint
-
Sternocleidomastoid
-
Stretching
-
Subscapularis
-
Temecula
-
TMJ
-
Trapezius
-
Uncategorized