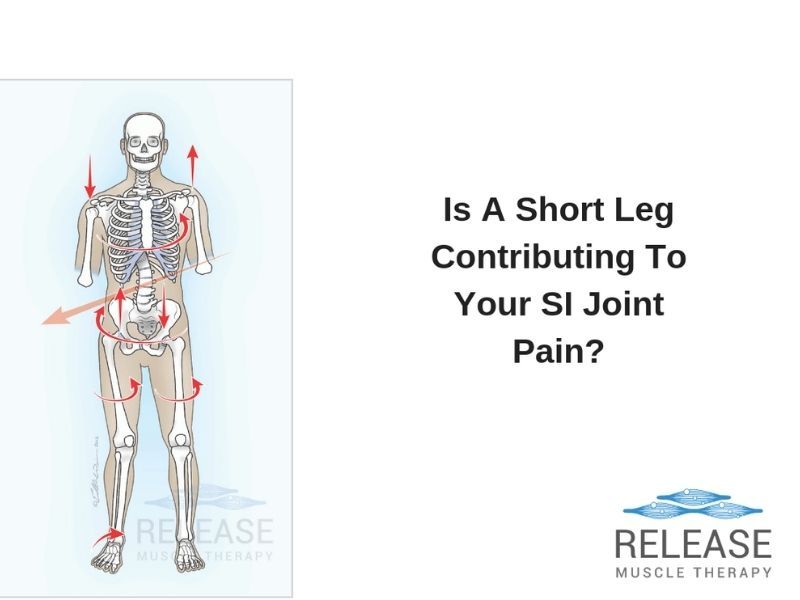
Is A Short-Leg Contributing To Your Sacroiliac Joint Pain?
A very important factor to rule out in chronic SI joint pain is that of a leg length discrepancy.
When the legs are not equal length, it can make the sacral base un-level, thus contributing to stress and strain at the sacroiliac joints and lower lumbar spine.
There are 2 different types of leg length issues that you should know about:

1. Anatomical Leg Length Discrepancy
This refers to when one leg is actually shorter than the other. This can be a result of injury to the joints/bones, or what you were just born with. The truth is that this type of leg length issue is very rare!

2. Functional Leg Length Discrepancy
This type is usually caused by muscle and joint imbalances, which upon correction, the leg length is restored. This is the MOST common type of leg length issue seen.
How To Test For The Two Types Of Leg Length Discrepancies
In this video, John Gibbons explains a simple test that can be used to assess leg length variation.
If a true anatomical leg length discrepancy is suspected, a full length X-ray may need to be performed to confirm.
How To Fix Functional Leg Length Discrepancy
Since functional leg length findings are associated to muscle and joint issues, they must be addressed by resolving these imbalances.
For instance, excess anterior pelvic tilt is a VERY common finding in SI joint-based imbalances and leg length discrepancy.
In the video above, I talk about the most common causes for excess anterior pelvic tilt, which include short/tight hip flexor and lower back muscles, and long/weak hip extensors and abdominals.