Plantar Fasciitis | Essential Guide To Relief
Nothing gets between you and having a great day than a stabbing pain that keeps you from moving around. Specifically, a pain that originates at the bottom of your heel.
If you are experiencing pain, it would be wise to first visit your doctor or podiatrist for a proper diagnosis and a recommended treatment plan before going any further.
The pain may originate from your plantar fascia ligament. Usually, exerting too much pressure on the area results in irritated fascia, making it inflamed, which could be the primary reason for your foot pain.
Based on your unique case and the extent of the inflammation, your doctor may recommend temporary immobilization or specific non-surgical treatment. There are a lot of options in this area but at the top of the list is a physical therapy program, which may include a variety of modalities including exercises, stretching, orthotics, or other tools to help alleviate discomfort like a massage gun, or kinesiology tape.
However, in severe cases, your doctor may also recommend surgical procedures, depending on the extent of your condition.
In this article, we’ll delve deeper into plantar fasciitis⸺ a very common painful foot condition, its causes, symptoms, treatment options, plus how to prevent it, and what to avoid when you have the condition.
What Is Plantar Fasciitis
Plantar fasciitis is a painful foot condition highlighted by a sharp stabbing pain originating at the bottom of the heel (but it may present more toward the forefoot in some cases).
Usually, this pain occurs when the plantar fascia is irritated, thanks to the combination of precipitating factors and the wear and tear of daily life. Plantar fascia is a weblike ligament that is thick and runs from the heel of your foot to the toes.
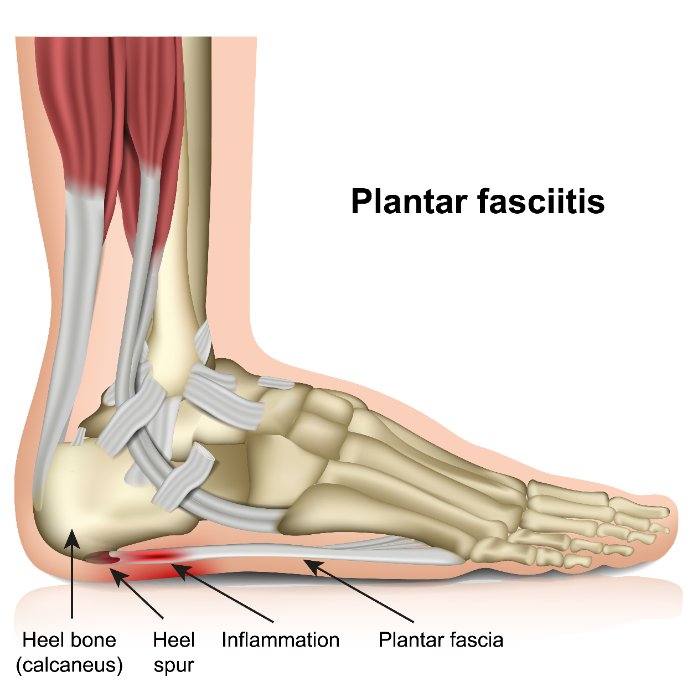
The plantar fascia ligament supports the foot’s arch to help you walk. It also absorbs shock.
When you place weight on your foot, such as during prolonged standing, regular walking, running, or weight bearing, over time, that puts stress and tension on the plantar fascia, which is completely normal.
However, the plantar fascia can lose its resilience or elasticity, which causes it to tear or become irritated with daily activity.
Symptoms of Plantar Fasciitis
Many patients who present with plantar fasciitis complain about pain in the bottom of the heel or occasionally in the midfoot area. Plantar fasciitis usually occurs in one foot, but sometimes the condition can affect both feet.
Plantar fasciitis pain can come and go, but the worst pain occurs with the first few steps when you get out of bed. This is due to the position of the feet during sleep, as they are in plantar flexion (think calf raise).
As you stay on your feet, the plantar heel pain usually reduces but can reoccur when you suddenly stand after sitting for too long or standing for too long.
The heel pain may also intensify on bare feet or when you wear worn-out shoes that offer no heel and/or arch support.
The pain can evolve gradually, and as the condition worsens, it will move from dull to sharp. Although some people describe the pain as a burning ache starting at the foot’s heel and spreading throughout the bottom of the foot.
Causes and Risk Factors of Plantar Fasciitis
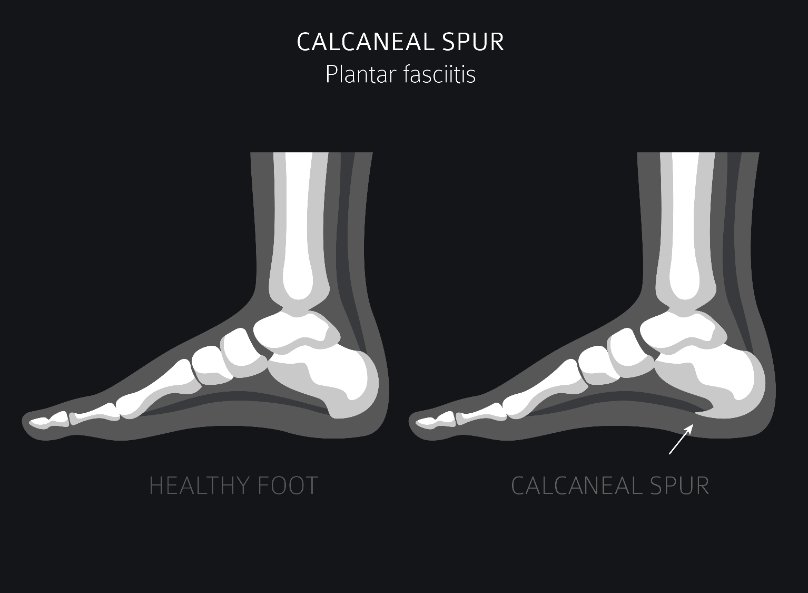
A common misconception has been that heel spurs or bone spurs could cause plantar fasciitis. However, that misconception has now been disputed.
Yes, heel spurs can exacerbate plantar fasciitis as they also cause stress on foot ligaments, but it’s also possible the heel spur is caused by the plantar fascia tension. Regardless, focusing on the heel spur itself may miss the additional factors that are contributing to the pain.
Many factors can predispose you to develop plantar fasciitis, including your foot structure, age, gender, or level of physical activity (more on this below).
Plantar fasciitis commonly occurs in women more than in men. In addition, pregnant women, especially during the later stages, may experience bouts of heel pain.
Plantar Fasciitis Risk Factors
Sometimes plantar fasciitis can develop without any apparent cause. However, certain factors can increase your probability of developing heel pain. Such factors include:
- Obesity and weight. The excess weight caused by sudden weight gain or obesity increases pressure on the foot ligaments.
- High-impact training. Aerobic dancers, ballerinas, runners, and high-impact athletes do intense exercises that place a lot of stress on the feet muscles and support structures, and can result in severe pain in the heel.
- Active jobs that keep you on your feet. Doctors, factory workers, waiters, barbers, and teachers spend long periods on their feet, either walking or standing.
- Foot structure (pes planus). Flat feet or pes planus occur because of weak ligaments. Pes planus make the plantar fascia and other tendons in the foot work harder to support the foot, which may cause the fascia to wear and tear much faster.
- Tight Achilles tendon. Your Achilles tendons connect your calf muscles to your heel. Tightness in the Achilles tendon can reduce ankle flexibility (dorsiflexion) and add more pressure on the connective tissues.
- When you often wear shoes that are old and need to be replaced. Wearing supportive shoes with orthotics (shoe inserts) can relieve pressure on your plantar fasciitis muscles, mitigating the development of heel pain. However, soft soles and shoes that have too many miles on them have poor arch support.
- Reduced ankle dorsiflexion due to lack of joint mobility and/or calf muscle shortness.

Complications That Can Result From Plantar Fasciitis
Not treating plantar fasciitis can result in chronic heel pain that can keep you from participating in regular activities, lowering your quality of life, and ultimately your health.
Patients with plantar fasciitis, like any other group dealing with chronic pain may also deal with increased anxiety and risk of depression.
Chronic pain can also make you change your walking style potentially leading to back, hip, knee, and foot issues.
How Doctors Diagnose Plantar Fasciitis
If you are experiencing plantar fasciitis and feel pain that is not resolving, consult your podiatrist for proper diagnosis and treatment. While at the doctor’s office, they will take an appropriate medical history, and perform a few checks to confirm that your foot pain is caused by plantar fasciitis and not any other conditions with similar symptoms.
Treatment of plantar fasciitis should be multidisciplinary, so other practitioners may need to be consulted to get a full understanding of the factors contributing to your case.
Physical Examination
During the physical examination, your doctor will check for:
- Muscle tone
- Balance
- Coordination
- Tenderness
Image Testing
Your doctor may perform imaging tests to identify the cause of your heel pain.
An X-ray will rule out a stress fracture. An MRI will show swelling or thickening of plantar fascia tissues, while ultrasound imaging will identify the thickening or calcification of any tissues. They can also check for the presence of heel spurs.
How Plantar Fasciitis Is Treated
There are a number of options for plantar fasciitis treatment. Home therapies such as night splints, heel cups, icing, and anti-inflammatory drugs are usually the first things you see online when searching for plantar fasciitis relief, but none offer the “magic bullet” for this problem.
Let’s dig into plantar fasciitis treatment options a bit more.
Non-Surgical Treatment for Plantar Fasciitis
Physical Therapy
Your therapist can recommend stretches for your Achilles tendon and heel ligament to relieve pressure off relevant tissues.
They will also guide you on exercises that strengthen the right muscles to lessen the load on the irritated fascia. Graston technique also seems to be quite popular amongst therapists as well for treating the soft tissues of the foot.
Plantar fasciitis can improve quite a bit as a result of strengthening these muscles in some people. Others may need much more.
Stretching Exercises
Plantar fasciitis leads to reduced ankle flexibility, which in turn leads to alteration in weight-bearing in the foot, putting more pressure on the plantar fascia ligament. Tight muscles additionally may be either a contributing factor OR the result of pain, but regardless they are an important factor to address even if they are not the cause of plantar fasciitis.
Tight calf muscles can pull on the Achilles tendons and may be a contributing factor in heel pain. Gently stretching your calf muscle can help loosen the muscle and reduce pain. The key is to start slowly, otherwise it can result in making the pain worse.
When you perform the best plantar fasciitis stretches consistently, you can expect significant improvement in just three months. Research shows plantar fasciitis improves fairly consistently with adherence to an appropriate stretching program.
The stretches work so well because they alleviate tension in the calf and lower foot muscles leading to greater flexibility and a reduction in heel pain.. Calf stretching has additional benefits to the overall muscle balance of the lower extremity as well.
Some individuals may benefit from wearing a night splint, which is meant to passively stretch the tissues and reduce morning plantar heel pain.
Plantar Fasciitis Exercises
With a mild case of plantar fasciitis, general stretches for plantar fasciitis will get you well on your way to recovery.
However, with severe plantar fasciitis, you may need a more precise exercise outline and information about which exercise to avoid so as not to exacerbate your painful heel condition.
Before you begin your exercise regime for plantar fasciitis, you’ll need to take a break from any significant activities that apply pressure to your plantar fascia. This can include running, standing for too long, or any daily activity that requires being on your feet for too long.
When you’re starting your plantar fasciitis exercise, start slow and build your way up.
When you eventually get back on your feet, be sure to have supportive shoes. Night splints may also help fasten the recovery process.
With exercises, symptoms may take weeks or even months to improve. Generally, the longer you have experienced the symptoms or the more chronic your condition, the longer the span of the time it takes to see a good response.
Plantar Fasciitis Exercises To Avoid
There are exercises that can worsen your painful foot condition, so we need to make sure we cover plantar fasciitis exercises to avoid:
- Running and jogging. Repeated stumping of the foot on the ground with running and jogging puts a lot of strain on your fascia and foot ligament.
- Burpees. Burpees or squat thrusts apply a lot of pressure to the fascia and heel ligament as you drop to a squat, shift to a plant, then jump back into a squatting position before standing.
- Aerobics and cardio dancing. The quick footwork, jumping, hopping, and the amount of time you spend on your feet while doing cardio and aerobic dancing leads to faster degradation of your fascia and heel ligament, causing inflammation and eventually pain.
- High-impact team sports. Sports like basketball and football involve a lot of running and jumping, which can cause a tear in the ligament.
- Plyometrics. Jumping trains put the worst strain on your fascia ligament. A sudden impact jolt can easily tear your fascia ligaments, leading to severe pain.
You don’t necessarily need to stop exercising after developing plantar fasciitis. However, you should consult your doctor first beforehand to see if there are any specific recommendations on what to do/not to do.
This is because incorrectly exercising the areas may lead to a flare-up or worsening of plantar fasciitis.
With that said, it’s still possible to get your workout in or burn calories without putting strain on your fascia and heel.
A few alternatives to high-impact exercises come in handy here. For example, you can opt for power walking in the pool, swimming, or even rowing instead of jogging or running.
A plantar fasciitis-friendly alternative to burpees would be performing the squats without jumping and doing the planks on your knees.
The point is, there are many ways to get and stay fit without placing unnecessary strain on your already aggravated tissues.
Icing and Medication
Putting ice on the painful heel several times daily may help with inflammation and pain relief. A popular way to do this is to roll on a frozen water bottle.
It’s common to reach for the nonsteroidal anti-inflammatory drugs (such as ibuprofen) to help with pain management, but there is strong evidence that chronic plantar fasciitis is not a true inflammatory condition, but more like tendinosis. This is why you often come across the term “plantar fasciopathy”. In this case, these drugs don’t make sense to use!
Surgical Treatment
Your doctor will only recommend surgery in case of severe pain that lasts more than six to 12 months or if all other treatment options fail.
Surgery is generally considered a last resort, because it is not without risks and it may not work for many patients with plantar fasciitis. Nonsurgical treatment options should always be exhausted when appropriate.
Plantar Fascia Release
In plantar fascia release, the orthopedic surgeon will cut a part of the plantar fascia ligament or entirely detach it from the heel bone.
This should relieve tension in the area and reduce inflammation. However, because the surgery may involve entirely detaching the plantar fascia ligament from the heel bone, it may result in loss of full function of the foot due to a weakened foot arch.
Relief is not guaranteed either. I have personally seen a number of clients that have the same pain after the procedure.
Gastrocnemius Recession
With gastrocnemius recession surgery, your orthopedic surgeon lengthens the gastroc tendon, a part of the Achilles tendon, so the ankle can be more flexible and move about easily. This results in reduced stress on the plantar fascia.
The success of this is likely going to be correlated with the degree of involvement of the achilles tendon.
Other Non-Surgical Remedies for Plantar Fasciitis
Often, the conservative treatment for plantar fasciitis is the first-way heel pain is managed.
Outside of the usual stretching and exercise protocols, there are different measures that can be taken, some more evidence backed, while others purely anecdotal, but seem to work for some people.
Cortisone Injections
Although injections are a common approach to treat plantar fasciitis, they are not without scrutiny. Some experts believe steroid injections can increase the risk of plantar fascia rupture. Torn fascia obviously would be a disastrous outcome, so this one may be only reserved for those who are desperate for relief.
Massage Guns For Plantar Fasciitis

I’m mentioning this one because these massage tools are all-the-rage right now and sold as a cure for virtually everything. Clearly they are not, but there may be some short term benefit if you already have one.
A massage gun on your foot can help alleviate plantar fascia symptoms because of the vibration the device produces, which can contribute to “novel stimulation” and a temporary interruption of pain perception.
The vibration helps with fluid and blood flow in the foot muscles. As the massage gun vibrates, more nutrient-rich blood flows to the affected area, supplying all the compounds necessary for the healing process to begin.
Over time, consistent massaging of the tight calf muscles and the fascia can reduce nerve sensitivity, increase flexibility and mobility, and reduce tightness in the plantar fascia muscles of the foot.
It would help to choose the right massage gun for your painful foot condition for the best possible results.
Kinesiology Tape For Plantar Fasciitis
Along with exercise, your therapist may also recommend traditional Low Dye taping, or kinesiology taping on the affected foot area to help with the pain. This is a common and widely used treatment of plantar fasciitis.
A 2015 study revealed that taping your foot offers temporary pain relief from plantar fasciitis.
Kinesiology tape is another option which can also help reduce some loading, but also allow less restricted movement (which may defeat the purpose for some people!).
Your physical therapist may also recommend taping other muscles around your ankle and foot to control the activity of muscles contributing to your plantar fasciitis.
Here are the primary functions of taping for plantar fasciitis:
- Take the pressure off of your plantar tissues (unloading)
- Decrease the pain
- Help the muscles surrounding your foot to provide more support
- Support the foot’s natural arch
Sport or Kinesiology tapes (KT taping) are usually safe and do not cause any reactions. But if you begin to itch or notice redness in the area with the tape, it may indicate an allergic reaction. Gently remove the tape and consult your doctor or therapist for another option.
Self Massage For Plantar Fasciitis

Additional therapy, like massage therapy, can help with pain relief. With this type of therapy, the brain is given something else to focus on, therefore, it shifts focus from pain. On top of that, massage relaxes the tight and painful muscles, encouraging blood flow and may reduce the effects of acute inflammation.
If you are not able to consistently see a professional massage therapist, self-massage is the next best thing.
Self-massage, together with stretches and exercises, can be effective in curbing plantar fasciitis before it becomes chronic.
Self-massage techniques for chronic plantar fasciitis should feel good or just a little uncomfortable but not too painful. It would be best to start with soft presses against your foot and increase the pressure as the nerve sensitivity improves.
Targeting trigger points may be an additional benefit.
Because plantar fasciitis pain is usually intense with your first step out of bed, do some self-massage techniques while you’re still in bed before you get up.
This will warm your feet, get the blood flowing, and alleviate tension while prepping your foot to bear your full weight on standing.
Orthotics to Help With Pain
Orthotics are custom-made support devices sometimes prescribed by doctors to help with foot or back problems, but are even more commonly used in the treatment of plantar fasciitis.
The devices are designed according to limb contour to either reduce motion or stabilize the limb, depending on the specific treatment application.
For plantar fasciitis, your doctor may recommend devices such as orthotic inserts, wearing night splints, heel cups, or specific shoes specifically designed to support the foot and to reduce chronic plantar fasciitis pain and the effect of heel spurs.
Your podiatrist may recommend orthotics in conjunction with other treatments, such as taking nonsteroidal anti-inflammatory drugs (NSAIDs), leg braces, or physical therapy.
So how do orthotics work?
First, the devices work to reposition your feet correctly. For example, when your feet overpronate, they roll inward as you walk. For some patients with plantar fasciitis, this can result in a reduction in acute irritation due to the repetitive stimulation of the painful area.
The edge of your heel gets to the ground first, then the rest of the foot rolls inward towards the arch.
This phenomenon is also common in people with flat feet. Orthotic devices and/or arch supports provide support to the arch to try and correct this phenomenon. Orthotics may also offer cushioning and additional support in crucial foot areas such as the ball or heel of the foot.
Orthotics are custom-made, so they focus on the individual’s footwear needs. Here are a few types of orthotics for feet:
- Full shoe inserts
- Small heel inserts for the back cup of the shoes which can reduce heel pain discomfort
- Ankle foot orthotics that include an upright part extending from the heel upward to round the calf area, and a shoe insert.
Extracorporeal Shock Wave Therapy
Extracorporeal shockwave therapy has shown promise in recent research. This therapy involves using a tool to send shockwaves into the plantar fascia to trigger healing.
Only time will tell is this unique therapy pans out, but it is an option for particularly stubborn cases.
How Long Does It Take To Recover From Plantar Fasciitis?
Most people have reported that simple cases of plantar fasciitis symptoms or heel pain usually go away after a few months of home remedies which can include resting, stretching, icing, and using the modalities listed above.
Proper REST is essential for many people, but this advice is often only partially adhered to. Oftentimes when someone feels slightly better, they quickly start increasing activity levels only to get setback with another bout of pain.
Start simple first. Things like a night splint to stretch lower leg muscles could provide a great result, and avoid jumping to the most aggressive approach before doing the basics.
In chronic cases, this condition can last on average around a year, and for some people, much longer.
How to Prevent Plantar Fasciitis
Making a few positive lifestyle changes can keep plantar fasciitis at bay.
Avoid shoes that aren’t supportive and find alternatives that offer excellent arch supports.
It’s also good to regularly replace your exercise shoes. The wearing time for athletic shoes is about 400 to 500 miles. After that, it would be best to get a new pair.
Stretching your plantar fascia, calf muscles, and Achilles tendons is also a great idea before any workout sessions. And try to limit your high-impact exercise. Instead, opt for low-impact activities like swimming or cycling.
Always perform an appropriate ramp up of new activities. One of the common triggers for any type of heel pain or tendonitis issue is a sudden increase in activity levels and/or intensity. Starting a new job that requires long periods of standing is something to avoid as well!
Get Your Life Back From Plantar Fasciitis.
Plantar fasciitis affects 85 percent of Americans annually. Unfortunately, most people experiencing these symptoms do not seek proper medical attention to manage the condition.
Notably, plantar fasciitis can lead to severe ongoing pain if not adequately treated. Therefore, visit your podiatrist and discuss the learnings from this post to see what’s right for you.
Sam Visnic
Most Popular Posts
Categories
- Deep Gluteal Pain Syndrome (8)
- Deltoids (2)
- Foam Rolling (2)
- Glutes (9)
- Hamstrings (5)
- Hypnosis for Pain (3)
- Lats (2)
- Levator Scapulae (4)
- Lifestyle (8)
- Massage Therapy (39)
- Mobility (21)
- Movement and Exercise (19)
- Muscles (22)
- Nutrition (2)
- Obliques (1)
- Pain (25)
- Pectorals (3)
- Piriformis (3)
- Plantar Fasciitis (11)
- Psoas (11)
- Quadratus Lumborum (3)
- Quadriceps (2)
- Rhomboids (3)
- Sciatica (1)
- Serratus Anterior (1)
- SI Joint (14)
- Sternocleidomastoid (1)
- Stretching (18)
- Subscapularis (1)
- TMJ (2)
- Trapezius (1)
- Uncategorized (12)